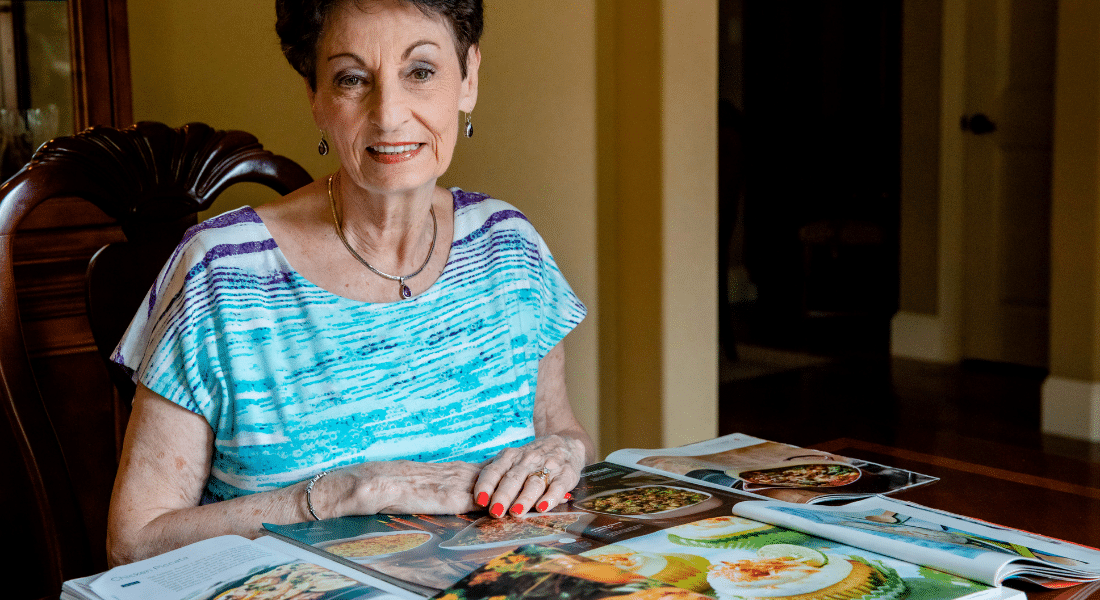
Patricia French loves good food and cooks a great deal, but until recently, her gastroesophageal reflux disease (GERD) made the act of eating more of a logistical challenge than a pleasurable experience.
“The problem had nothing to do with spicy foods or what I was eating. It was that I was eating at all,” says the 79-year-old retired real estate agent, who couldn’t eat anything at night because of her painful symptoms.
It wasn’t until Patricia sought help from the Heartburn Treatment Center at Methodist Mansfield Medical Center and opted for a robotics-assisted surgery that she was able to enjoy food again.
“I was really blessed by the surgery and the efficiency of it all,” she says. “I eat everything, whenever I want, as late as I want now.”

Patricia once had to take a regimen of medications to eat — but not anymore
A HINDRANCE TO A FULL LIFE
For years, Patricia’s condition took a toll on her active lifestyle. She and her husband regularly cruised to the Mediterranean, but she had to request early meals just to get through the night. Even at home, Patricia took acid reflux medication every day for GERD and couldn’t eat anything after 5:30 p.m.
“If I did, I would feel it,” she says. “That terrible burning was painful.”
As Patricia’s symptoms got worse and her medication less effective, she decided to see a professional for help. She turned to Sunitha Pudhota, MD, gastroenterologist on the medical staff at Methodist Mansfield.
Dr. Pudhota ran diagnostic tests to track the movement of food through Patricia’s esophagus and measure her acid reflux. The results showed that Patricia had poor esophageal motility and a hiatal hernia, which occurs when the upper part of the stomach pushes into the chest through an opening in the diaphragm.
Knowing Patricia would need surgery, Dr. Pudhota referred her to Jeremy Parcells, MD, a general and bariatric surgeon on the hospital’s medical staff.
“Heartburn is a disease that affects about 20% of the population,” Dr. Parcells says. “What you really want is a nice one-way street. You want to be able to eat, have food go down, and not come back up. When things are out of position and not where they’re supposed to be, it starts to kind of mess with what’s a really elegant system.”
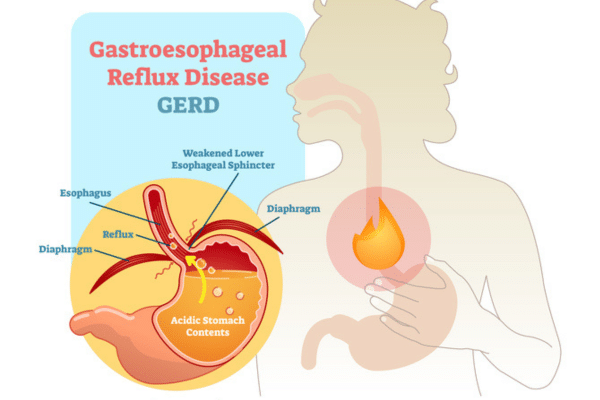
With GERD, food and acid escape the stomach into the esophagus.
ROBOTICS-ASSISTED SURGERY
Dr. Parcells told Patricia that in order to repair her hiatal hernia and resolve her GERD issues, he had to perform a Toupet fundoplication, a surgical technique where the upper section of the stomach — called the fundus — is folded and stitched around the esophageal sphincter to reinforce that “one-way street” and help prevent food and acid from moving up the esophagus.
“He explained to me exactly what the problem was and gave me a copy of every test. I never had to ask for anything,” Patricia says.
On the day of her procedure, Patricia checked into Methodist Mansfield, the same place where she had her testing done.
“It’s all right there. It’s a one-stop shop. That’s what’s so nice about it,” she says.
Dr. Parcells used the robotic da Vinci Surgical System to perform the operation. The advanced technology provided him with better visualization and allowed for more precise movements than conventional laparoscopic approaches.
“You go from having normal 2D vision to actually having 3D vision,” Dr. Parcells explains. “The instruments provide vastly superior degrees of freedom and motion. You get the best possible outcome for a patient when you combine a proper workup with someone who’s an experienced expert in this kind of surgery.”
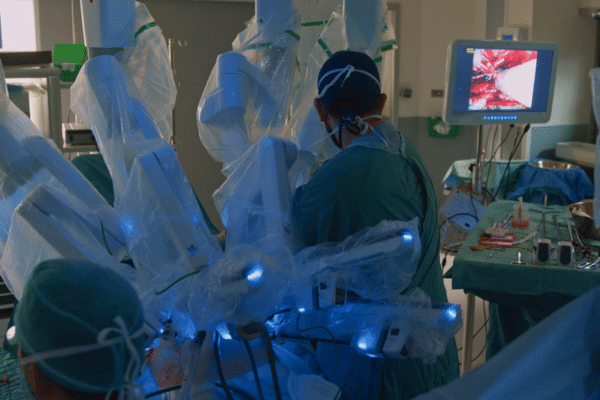
With the surgical robot, a doctor is always in control but benefits from extra precision and a better view.
EATING WELL AGAIN AT ANY TIME
Within hours of her procedure, Patricia was already home and on the path toward recovery.
“I had a whole packet of information as to what I could eat for the next few weeks, it was very complete. But if I ever had a question, I could call and a nurse would always have an answer for me,” she says.
Patricia followed a primarily liquid diet to start and had routine follow-up visits to monitor her health. But before long, she was back in the kitchen — and back on the cruise ship — able to enjoy food again.
“I can eat at 11 o’clock at night if I want to, and I’d have no problem — no medication necessary,” she says. “Now, whenever we travel, we just do what we want, eat what we want, and go where we want. It just worked out beautifully. I’m so thankful. I’m a happy camper.”