In a state with a never-ending allergy season, Texans are no strangers to “cedar fever.” But with COVID-19 cases on the rise again, it can be hard to tell the difference between an allergic reaction to tree pollen and something more serious.
“Cedar fever is common in Texas,” says Jagadeshwar Reddy, MD, pulmonologist on the medical staff at Methodist Dallas Medical Center. “There are usually spikes in pollen counts in December, January, and even February when the cedar trees pollinate.”
For many people, these irritants trigger itchy and watery eyes and a tickle in their noses.
“But for some, the pollen can trigger a strong immune response, and some symptoms may be the same as those of COVID-19,” Dr. Reddy says.
That includes a runny nose and sneezing, which are among the most common symptoms associated with JN.1, the Omicron variant behind a recent uptick in cases. What’s more, Omicron may not cause a loss of smell or taste, a hallmark of early strains.
“Omicron is less likely to affect taste and smell than the prior variants,” Dr. Reddy says. “But that doesn’t mean Omicron has no effect on those senses.”

COVID-19 VS. CEDAR FEVER
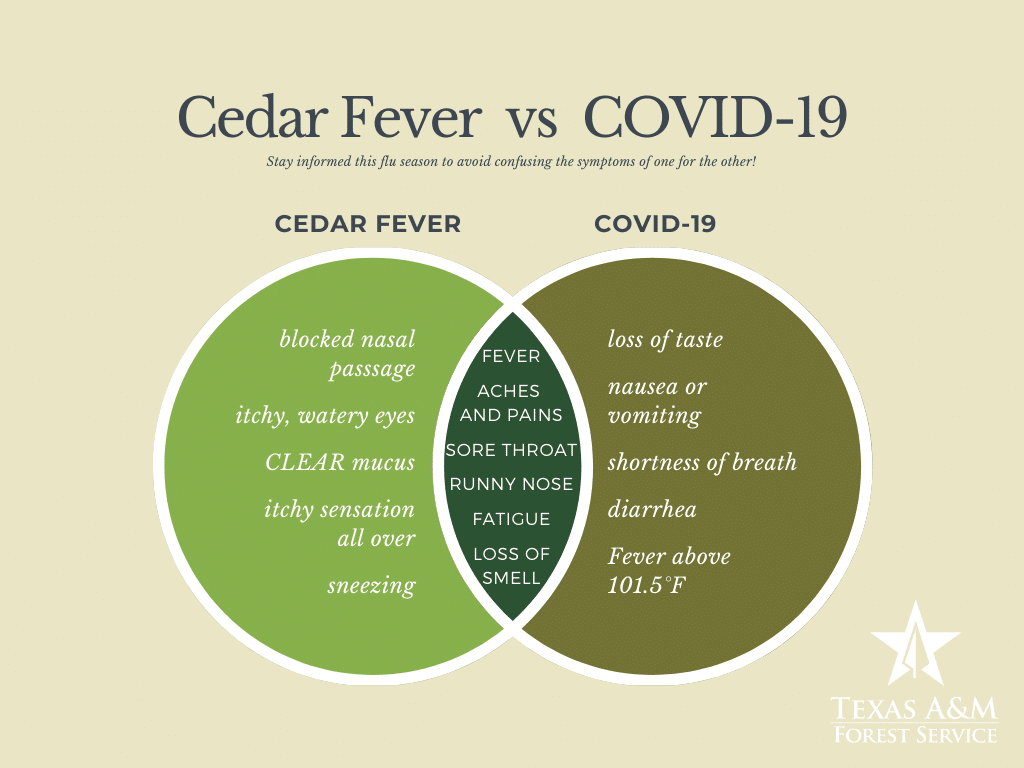
Even longtime allergy sufferers may have trouble distinguishing between the familiar symptoms of cedar fever and the telltale signs of COVID-19.
“With allergies, you may experience a headache, a cough, fatigue, a sore throat, and runny nose,” Dr. Reddy says. “These are also possible COVID-19 symptoms.”
The key symptoms that set COVID-19 apart, Dr. Reddy says, are fevers of over 100 degrees, chills, body aches, and gastrointestinal symptoms like vomiting, diarrhea, and nausea.
Another sure sign that the virus is what ails you: Because COVID-19 is so contagious, everyone in your home may be feeling ill around the same time.
“If multiple members in the household or close contacts are having similar symptoms,” he says, “then COVID-19 should be considered as highly likely.”
If it is COVID-19, Dr. Reddy suggests that whoever is sick quarantine and seek medical attention, especially if they are high-risk patients who would benefit from an anti-viral medication.
“For outpatient treatment, Paxlovid is effective in reducing severity and duration of symptoms,” he says.
However, the anti-viral pill should be taken within five days of symptom onset, the earlier in the infection the better. That’s because it interferes with the virus’s ability to replicate in the body, and it may even help prevent “long COVID.”
ALLERGY REMEDIES
Like most allergies, cedar fever typically doesn’t require medical attention unless it triggers an asthma attack or spirals into a sinus infection, Dr. Reddy says. Most of the time symptoms can be treated with over-the-counter or prescription medicine, such as antihistamines and corticosteroid nasal sprays.
“Staying inside also helps, especially when it’s windy,” Dr. Reddy says.
Indoors, he recommends maintaining a clean household and practicing good personal hygiene. Showering, swapping out pillowcases and bedding regularly, and changing clothes can clear lingering particles that inflame allergies.
Neti pots, air humidifiers, and special air filters for the home may also provide relief. High-efficiency particulate air (HEPA) filters are specially designed to keep out dust, pollen, and other irritants.
“Many of the guidelines meant to protect us from COVID-19 — wearing masks, staying home, washing our hands — also protect us from cedar fever and other allergies,” Dr. Reddy says.

PROTECTING YOUR HEALTH
Taking those extra precautions, whether it’s warding off allergens or getting a flu shot or a booster dose of the COVID-19 vaccines, may be more important than you think, especially with COVID-19 cases rising again.
“Whenever your body’s being strained by anything, you’re more likely to get a viral illness,” Dr. Reddy says.
If you’re not getting enough sleep, dealing with allergies, or feeling stressed, it can leave your body too battered to fight off an infection.
“Each time your body encounters these stressors, it weakens the immune system a bit,” he says. “So it’s really important to take preventive action. It can affect your immune health.”






