Irritable bowel syndrome is the most common diagnosis made by gastroenterologists, affecting 10% to 15% of the population, or 50 million people, but what causes IBS, and the connection between the two, has remained a mystery — at least until recently.
“We think IBS starts after certain types of infections in the GI tract,” says Jeffrey D. Linder, MD, gastroenterologist on the medical staff at Methodist Richardson Medical Center. “After the infection is gone, the IBS symptoms can linger for quite a long time — months or even years.”
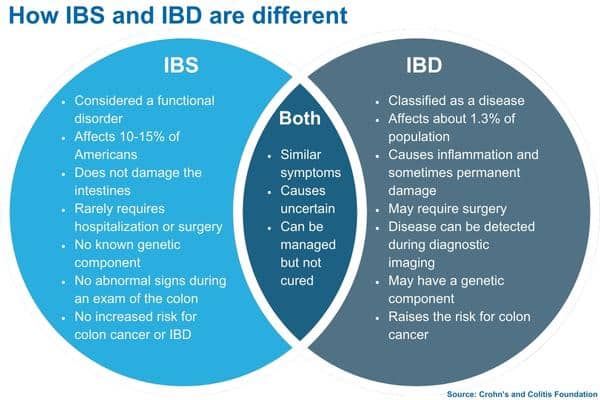
While it’s not a disease like Crohn’s or ulcerative colitis, IBS can share symptoms with these inflammatory bowel diseases (IBD). Shared symptoms include chronic abdominal pain and cramping, bloating and gassiness, nausea, and diarrhea or constipation.
IBS is what’s known as a functional disorder, so while it causes no damage to the bowel, it does disrupt its healthy function. It has been referred to as a “diagnosis of exclusion,” something a patient is diagnosed with when all the tests come back normal.
But ask any IBS patient and they will tell you they don’t feel normal. Sometimes they’re told it’s “all in their head,” but that doesn’t make their misery imaginary.
“Some IBS is anxiety related, and sometimes certain foods are a trigger,” Dr. Linder says. “We never know what has caused IBS in certain patients.”
But recent studies offer hope that researchers will find a biological explanation and, eventually, a solution to ease patients’ pain.
BRAIN-GUT CONNECTION
Stress can aggravate the symptoms of IBS because of the well-known connection between the brain and the gut. There’s a specific chemical that creates this link.
“Serotonin is a neurotransmitter that is key to depression and anxiety,” Dr. Linder says. “It also happens to be the same neurotransmitter our gut uses for pain reception.”
This connection, or axis, runs in both directions, Dr. Linder says, especially for patients whose digestive system is more sensitive to stimuli.
“Because of that, some GI conditions can cause us to be anxious,” he says, “and sometimes anxiety or excitement can give you a variety of GI symptoms.”
That’s why antidepressants and anxiety drugs are often prescribed to ease the symptoms, as are cognitive behavioral therapy, meditation, and other relaxation techniques.
Other patients find relief in exercise, from yoga to running, which helps relax the abdominal muscles and aids in digestion. Another technique, which can be practiced during any of these exercises, is called diaphragmatic breathing, or “belly breathing.” Think of it like the opposite of sucking in your gut, and you’ve got the right idea.
All of these methods can offer relief, although none is the surefire fix that IBS patients long for. But now that researchers are closing in on a cause, a solution may be on the horizon.

ARE ALLERGIES TO BLAME?
Another way people with IBS find relief is by restricting their diets. Often that means adopting an elimination diet to remove problem foods like dairy, gluten, and FODMAPs like beans, onions, and garlic, which are hard for the small intestine to absorb.
Some patients can trace a food allergy and the resulting IBS symptoms back to a stomach bug. Researchers now suspect these infections are what cause the digestive system to go haywire in the first place.
A June 2021 study published in the New England Journal of Medicine pointed to how a GI infection disrupts the intestinal lining that normally prevents allergens from being absorbed by the bowel. So a patient with IBS may lack this barrier, making their digestive system more sensitive to allergy-causing proteins.
In short, that means IBS and other functional GI disorders may originate with an allergy to certain foods that most people can eat without a problem. The solution could lie in an antihistamine targeting this overreaction, like the daily pills so many people take for seasonal allergies.
Another potential treatment may lie in medications, currently in Phase 3 trials, that target the white blood cells, known as “mast cells,” that cause an allergic reaction in the gut. Mast cells may be better known for the roles they play in asthma and hay fever.
HOW IBD DIFFERS FROM IBS
Before trying to relieve any of these symptoms, it’s important to understand the difference between IBS and IBD. When we call IBS a diagnosis of exclusion. It’s inflammatory bowel disease that a doctor is trying to exclude.
And then there are those patients who may suffer from both.
“Sometimes IBD and IBS can overlap,” Dr. Linder says, “and then we would treat both with different medicines.”
IBD comes in two forms: Crohn’s disease and ulcerative colitis. Both involve the chronic inflammation of the digestive tract. Blood in the stool is a telltale sign for both, but uncommon for IBS, Dr. Linder says.
“IBD is treated with anti-inflammatory medications that are released in the intestine,” Dr. Linder says. “Other medications we use are steroids, immunomodulators, and biologics.”
Another way IBD is different: the inflammation it causes can lead to a higher risk of colorectal cancer. That’s why it’s so important for patients living with Crohn’s or colitis to regularly consult with a GI doctor and schedule routine colonoscopies.
“The most important thing a person with IBD can do to reduce the risk is to see a gastroenterologist to manage their disease with medications,” Dr. Linder says. “The gastroenterologist can help get that person into a surveillance program.”






