The most common disease affecting the liver afflicts about 1 in 4 Americans, but too few people understand the risks of fatty liver disease.
“The presence of more than 5% to 10% fat of the liver’s weight causes inflammation, cell injury, and even cell death,” says Ashwini Mehta, DO, transplant hepatologist on the medical staff at Methodist Dallas Medical Center.
In many cases, alcohol abuse is to blame for this potentially life-threatening increase in fat content, but not always. Non-alcoholic fatty liver disease, which affects people who drink little to no alcohol, is the most common form of liver disease worldwide.
“About 1 in 5 people with this condition will get progressive fatty liver disease, which is commonly associated with obesity, type 2 diabetes, and high cholesterol,” Dr. Mehta says.
Here’s what else you should know about liver disease, a disease that claims about 50,000 American lives each year and about 2 million worldwide.
WHAT THE LIVER DOES
Weighing just over 3 pounds, the liver is the second largest organ after the skin and serves many functions that prove its worth as one of the body’s most important organs.
Among other functions, the liver filters bacteria and toxins from the blood, prevents infection, regulates blood clotting, and stores sugars, minerals, nutrients, and fats — too much of which can lead to steatosis, or fatty liver disease.
“The liver converts the nutrients in our diets into substances that the body can use,” Dr. Mehta says.
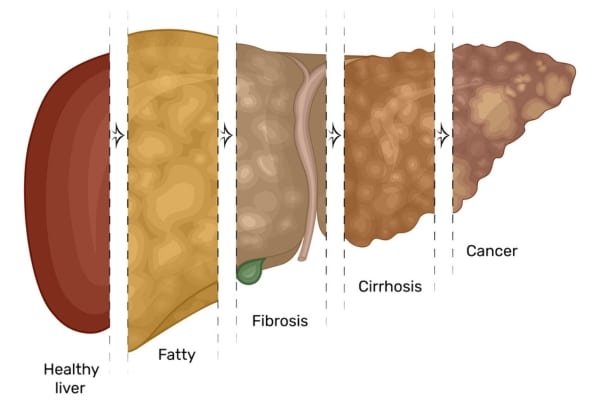
Taking care of the organ is paramount to avoid early-stage liver disease and the conditions it can lead to, such as hepatitis, inflammation of the liver; fibrosis, when the inflammation stiffens the liver; and cirrhosis, when scar tissue replaces healthy tissue.
While hepatitis and fibrosis are reversible, cirrhosis is not and can cause liver failure or liver cancer, both of which could require a transplant.
Although cirrhosis is often associated with alcohol abuse, many forms of liver disease can lead to late-stage liver disease, including non-alcoholic fatty liver disease.

NON-ALCOHOLIC FATTY LIVER
Non-alcoholic fatty liver disease is defined by an increased buildup of fat that is not associated with excessive alcohol use.
Often diagnosed in people who are overweight or obese, this disease can be serious, but it’s preventable and treatable when caught in its early stages.
There are usually no symptoms, although patients may feel fatigued or have pain in their right upper belly.
But when it develops into hepatitis or cirrhosis, symptoms can include itchy skin, swelling of the legs and abdomen, and yellowing of the skin and eyes, sometimes known as adult jaundice.
“About 5% of the 83 million Americans living with fatty liver will develop hepatitis,” Dr. Mehta says. “And 2%, or 3.3 million, will progress to cirrhosis.”
Risk factors go beyond being overweight or obese and include diabetes, high cholesterol, sleep apnea, living a sedentary lifestyle, and genetics.
“Race also seems to play a role,” Dr. Mehta says, “with Hispanics most at risk, followed by Caucasians and Asians.”

ALCOHOLIC FATTY LIVER
Excessive alcohol intake can lead to an array of health problems, including stroke, high blood pressure, and damage to the heart and pancreas.
Alcohol use disorder also happens to be the leading cause of liver disease in the U.S., and more specifically, alcoholic fatty liver disease.
“It’s the most frequently misused drug in the U.S.,” Dr. Mehta says, “and 15% of people with alcohol-use disorder will develop cirrhosis.”
Nearly two-thirds of American adults identify as moderate to excessive drinkers, and over 28 million men and women reported living with alcoholism in 2023, according to the National Survey on Drug Use and Health.
“Excessive drinking adds up to more than 14 drinks per week for men, and over seven drinks per week for women,” Dr. Mehta explains.

HOW TO REVERSE IT
There are many ways to keep your liver healthy and happy, such as staying current with age-related screening tests and checking your labs annually.
And if you’ve been diagnosed with fatty liver disease, reversing course involves making several lifestyle changes:
- Limit or avoid alcohol
- Lose weight
- Exercise regularly
- Limit intake of saturated and trans fats
Your diet is critical to preventing liver disease, so avoid foods that are high in added sugar, salt, refined carbohydrates, and saturated fat.
“Lean protein is a must,” Dr. Mehta says. “Choose chicken, fish, and plant-based proteins over red meat and fried foods.”
Finally, Dr. Mehta urges her patients to avoid taking herbal supplements because 20% of acute liver injury cases are caused by these unregulated pills.
“These cases can range from mild illnesses to liver failure, even requiring urgent transplant,” Dr. Mehta says. “Supplements are not regulated by the FDA, so their labels often have no meaning.”






