Dirk Huebl doesn’t remember much about his month-long stay at Methodist Mansfield Medical Center, but his wife knows all he’s overcome, from a brain hemorrhage to cardiac arrest.
“Once he started improving, it seemed like it was very quick,” Barbara Huebl says. “He returned literally from death’s door.”
What began as a bad headache in May 2023 led to a trip to the emergency room followed by surgery and a year of physical and occupational therapies. And while Dirk’s memories of that ordeal are fleeting, he will never forget those who saved him, a team led by Richard Meyrat, MD, medical director of neurosurgery at Methodist Mansfield.
“I’m very, very grateful for the care I received at Methodist Mansfield,” says the 58-year-old financial fraud analyst from Burleson, “and I’m thankful for having such a dedicated team of caregivers.”
Barbara remembers it all and couldn’t agree more.
“The neuro ICU nurses made you feel like they didn’t have a whole unit full of patients. They made you feel like you were the only one,” she says. “It felt like family.”
Patients like Dirk are now getting the dedicated neurological care they need in the new Neuro Critical Care Unit at Methodist Mansfield. Staffed by a team of neurosurgeons, critical-care nurses and rehabilitation specialists, the highly specialized 32-bed unit opened in 2024 to treat severe brain and spinal cord injuries, strokes, brain tumors, seizures, and other life threatening conditions. The Neuro Critical Care Unit at Methodist Mansfield was designed to care for patients just like Dirk.DEDICATED NEURO UNIT

BRAIN HEMATOMA
Dirk had been feeling poorly for a week in May 2023 when he awoke early one Saturday with a terrible headache.
When he couldn’t stand, his wife and their adult son helped him into the car and drove straight to Methodist Mansfield.
“I was not going to any other hospital,” Barbara says.
Once Dirk and Barbara got to the ER, she was terrified her husband was dying when his head rolled back and his eyes fell into a blank stare. Worse yet, his blood pressure was dangerously high: 220/117 mm Hg.
Scans revealed a blood clot in the middle of his cerebellum that was impeding fluid in his brain from draining into his spinal cord. That brain bleed, in turn, caused a buildup of cerebrospinal fluid that put pressure on his brain.
Weakened and immunocompromised by alcoholism, smoking, and poor nutrition, Dirk was admitted to the neuro trauma unit to be treated for the clot. But his prognosis was not good, especially after he suffered a cardiac arrest.
“His body basically fell apart, involving almost every organ system — lungs, heart, brain, circulation,” Dr. Meyrat says.
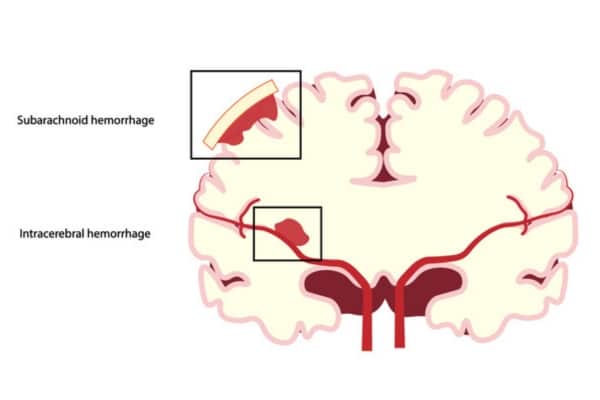
Dirk’s brain bleed was subarachnoid, meaning it was between his brain and the membrane surrounding it.
CARDIAC ARREST
When Dirk’s condition didn’t improve, Dr. Meyrat performed a ventriculostomy, drilling a hole above his right eye just behind the hairline, and placed a catheter to drain the excess fluid.
Dirk improved briefly but then suffered from a lack of oxygen, requiring him to be placed on a ventilator. He would also need a feeding tube and tracheostomy to prevent his larynx from being damaged. Again, he began to recover, but suddenly, Dirk went into cardiac arrest.
Fortunately, the neuro team reacted at lightning speed and was able to revive him.
“We left him on the ventilator,” Dr. Meyrat says. “With nurturing and time, he got better. He had multiple organ issues, and they were all treated appropriately and aggressively.”
The hematoma in Dirk’s brain receded, and he was soon breathing on his own again, allowing him to move into a long-term acute-care hospital (LTACH).
“Methodist was phenomenal. There wasn’t a person there who wasn’t top-notch,” says Barbara, who was especially grateful for Nurse Practitioner Jason Brown. “He sat down with me and acted like he had all the time in the world.”

MEETING THE TEAM
Dr. Meyrat says many patients may not recognize how large and complex their healthcare team is, and how all those roles must work in concert to save a life.
“Every element is so important,“ he says, “from the nurses at the bedside to the nurse practitioners who are the face of the doctors busy in the operating room.“
Months after his hospital stay, Dirk recovered enough to visit Dr. Meyrat and the neuro team. It was like seeing them all for the first time.
“I really enjoyed meeting Dr. Meyrat and nurse practitioner Jason and the nurses who took care of me,” Dirk says.
Dirk is now back at work part-time in his longtime role as a senior fraud analyst. He’s even quit smoking and drinking, Barbara reports.
“He learned the hard way that he was not doing what he should have been doing,” she says. “That is a blessing in disguise.”






