Managing type 2 diabetes has gotten less difficult with technology like continuous glucose monitoring and insulin pumps and patches.
But there’s no substitute for regular exercise and focusing on proper nutrition, says Saleemah Fahmi, MD, endocrinologist on the medical staff at Methodist Charlton Medical Center.
“The biggest issue is that patients aren’t doing enough to get protein in the form of lean meats and fiber in the form of vegetables,” she says.
When you eat can be just as important as what you eat, especially for patients who take insulin or other diabetes medications. Don’t skip breakfast and try to eat the same amount of carbohydrates at the same time each day.
What’s more, diabetic patients can go into remission if they lose enough weight, whether through bariatric surgery or a new regime of weight-loss drugs.
Of course, blood sugar levels can go haywire for even the most diet-conscious patient, so Dr. Fahmi offered some tips to better manage diabetes.

1. MAKE EXERCISE ROUTINE
All patients with diabetes should find a way to get active on a routine basis, whether that’s a daily trip to the gym or walking the dogs once or twice a day.
“I suggest that patients do something regularly, preferably for 45 minutes, five days a week,” she says.
Aerobic exercise — those cardio workouts that get the heart pumping — is an excellent way to lower the glucose level in your blood.

2. PATCHES MAKE LIFE EASIER
Daily injections were once a way of life for millions of patients with type 2 diabetes, and then insulin pumps became commonplace.
Today, technology has condensed pumps to the size of a patch, some of which last up to three days, that work in conjunction with a smartphone app.
“These patches are just more convenient,” Dr. Fahmi says. “For patients with busy lifestyles, this is just a lot easier.”
Like pumps, these patches continuously supply insulin through a quick needle prick and can administer additional insulin before eating or as needed to correct blood sugar levels.

3. BE CAREFUL DURING PREGNANCY
For women who are expecting or considering having a baby, gestational diabetes is a growing concern because pregnancy causes drastic changes in the body’s hormones, including insulin.
Gestational diabetes can be dangerous for the baby and mother, especially when left untreated. It raises the risk of stillbirth and can be associated with high blood pressure during pregnancy, also known as preeclampsia.
Like other forms of the disease, gestational diabetes is manageable, especially with a good OB-GYN to help guide the way. And in many cases, it goes away after the baby is delivered.
4. PAY ATTENTION TO A1C
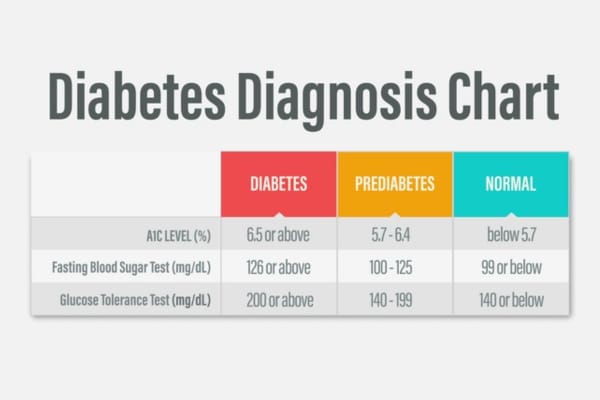
An A1C test is a simple blood test that averages your blood sugar level over the past two to three months. It’s commonly used to determine whether a patient has diabetes or is pre-diabetic. But for patients who are diabetic, it can help your healthcare team manage the disease and head off problems such as heart and kidney disease.
“Target levels should be somewhere between a 6.5 and a 7.5 because keeping them in this range helps a patient reduce the risk of complications, including heart issues, diabetic kidney disease, amputations, and infections such as pneumonia.”
If you have type 2 diabetes, it’s best to test your A1C twice a year, but anyone over age 45 should consider getting a baseline test, and younger adults might want to play it safe if they are overweight and have other risk factors for diabetes.

5. NEVER STOP LEARNING
Talking to your doctor on a regular basis is key to managing the disease, but so, too, is seeking out other support groups.
Workshops are held in-person and virtually at Methodist Charlton, among other hospitals, and feature the expertise of diabetes educators, physician champions, and registered dietitians.
Participants are also encouraged to discuss any challenges they are facing in managing their diabetes.
Making a commitment to educate yourself about the disease makes all the difference, Dr. Fahmi says.
“Ask about your target A1C score and blood-sugar levels, as well as how medication might be helping or hindering your health goals,” she says.






