When Kristin Booth suffered a sudden stroke in the middle of the night, she was rescued by the combined efforts of her husband, first responders, and the team at Methodist Mansfield Medical Center.
“Of all the things I thought might happen, that was not on my radar,” says the 45-year-old education consultant and mother of five. Fortunately, her husband, Aaron, was also awake and knew what to do.
Paramedics rushed Kristin to Methodist Mansfield, and the hospital’s alert system immediately notified a specialist, who was able to fix the problem less than three hours later.
“It was blessing after blessing in all of this,” Kristin says. “What if I hadn’t woken up? What if Aaron hadn’t woken up? What if Methodist Mansfield didn’t have this technology? I’m so lucky, so lucky.”
ALERT POWERED BY AI
In January, Kristin woke up at 3:30 a.m. to a shocking realization: She couldn’t move her right arm. Aaron also woke up then and recognized by Kristin’s slanted mouth and garbled words that she was having a stroke.
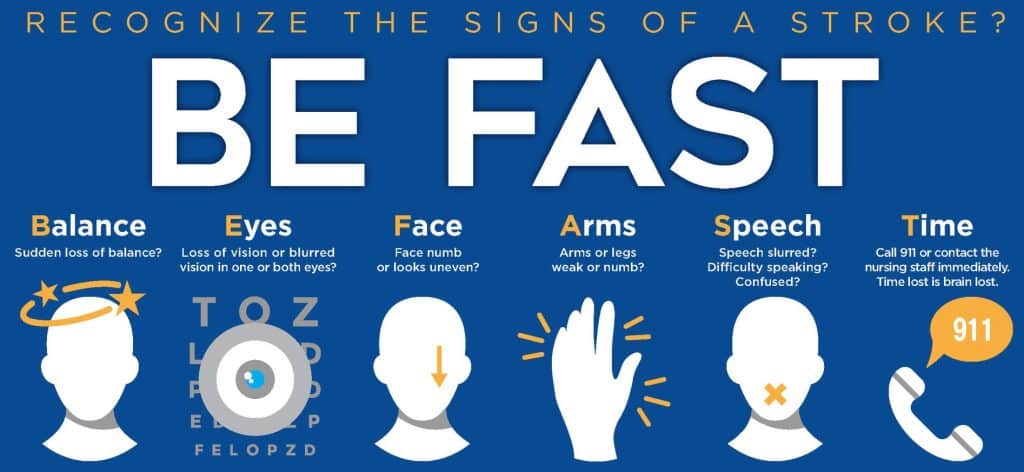
As the acronym BE FAST suggests, the most common stroke symptoms are balance issues, problems with the eyes or vision, numbness or weakness in the face and/or arms, and slurred speech. Any lost time before treatment could mean lost brain function, so it’s important to call 911 right away when these symptoms arise.
And that’s exactly what Aaron did. An ambulance took Kristin to Methodist Mansfield, where a team led by Matthew Fiesta, MD, neurointerventional radiology specialist on the hospital’s medical staff, jumped into action.
Dr. Fiesta credits a new emergency notification system for his speedy response: a smartphone app called Rapid, which uses artificial intelligence (AI) to send out alerts.
“Before, the routine would be a CT scan, then radiology reads it and the emergency department calls a neurologist, and they call a neurointerventionalist like myself,” Dr. Fiesta explains. “Today, an alarm goes off, and the app tells me that this is someone I can help. Instead of the emergency department calling me, I’m calling them and asking about the patient.”
Now stroke patients like Kristin can count on the new Neuro Critical Care Unit at Methodist Mansfield, which opened in January 2024 to treat a host of severe neurological issues from strokes and seizures to tumors and spinal injuries.
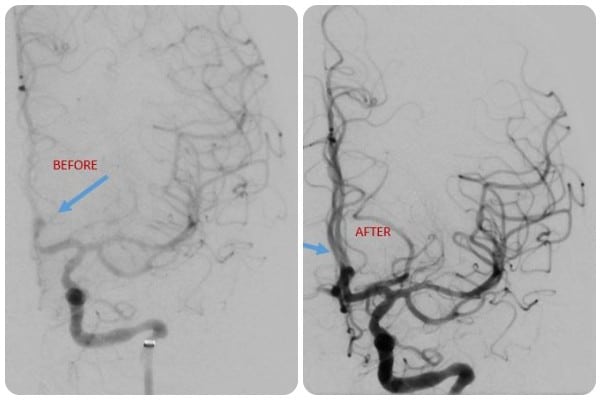
CT scans of Kristin’s brain show blood flow before the clot was removed (left) and afterward.
‘EVERYTHING CAME BACK’
A CT angiogram revealed a blood clot in Kristin’s left middle cerebral artery, the one most commonly involved in a severe stroke. On the scan, Dr. Fiesta could see how collateral blood flow was slowly detouring through an alternate pathway to reach the deprived brain tissue.
“The brain is in this metastable state where it’s getting enough blood flow to stay alive but not enough to be functional. The brain can only hold on for so long,” Dr. Fiesta explains. “That length of time is different for everybody. The main thing is don’t ignore the signs of stroke.”
Once Kristin was prepped at the hospital, Dr. Fiesta threaded a long, thin catheter through the femoral artery in Kristin’s thigh and gently guided it all the way to the clot in her brain. The catheter used suction to remove the clot and relieve the blockage.
“As soon as I woke up, I could feel my arm and leg normally again, and I could talk in a limited way,” Kristin says. “I’m so grateful that Methodist Mansfield has the technology to do that procedure because everything came back to me really quickly.”

Kristin feels blessed to spend more time with her family, including her husband Aaron.
TAKING CARE OF HERSELF
Over the weekend, Kristin worked with a nurse therapist in the intensive care unit to regain fluid speech and mobility, and on Sunday, she went home. Kristin felt ready to return to work only two weeks later, but her employer insisted she rest a bit longer.
“I don’t know how you thank people for saving your life,” Kristin reflects. “I have so much gratitude for Dr. Fiesta and all the doctors and nurses for giving me this time with my family. Every single person there was truly outstanding.”
Doctors believe the clot was created by a temporary fluttering of her heart known as atrial fibrillation. They are monitoring her heart and blood, and she’s taking a blood thinner to reduce blood clotting. Kristin suspects that stress and a less-than-healthy lifestyle were also contributing factors.
“I wore busyness like a badge of honor,” she admits. “I probably hadn’t slept more than five hours a night since I was in graduate school, and I didn’t exercise like I should have.”
Kristin now makes sure to sleep enough and exercise, and she’s drinking about two liters of water daily rather than just two cups of coffee like before.
“Taking care of myself is more important to me so I get to take care of others,” she says.






