Andrea Tubbs endured years of prolonged menstrual cycles and intense cramps, until 2022 when the pain pushed her to seek a surgical solution for her uterine fibroids at Methodist Charlton Medical Center.
“I was in the tub working with my laptop on the edge because I was in so much pain for weeks at a time,” says the 45-year-old from Cedar Hill, who found that soaking in Epsom salt provided temporary relief for the benign tumors growing in her uterus. “After a couple of months in a row like that, I was in tears.”
With her quality of life suffering, the mother of three who works as an administrator with the Federal Emergency Management Agency felt compelled to consider more drastic treatment options.
Andrea ultimately decided to have a hysterectomy after a discussion with her physician, DeShawndranique Gray, MD, OB-GYN on the medical staff at Methodist Charlton. That choice was validated by the quality of care she received at the hospital, she says.
“The nurses and support staff were fabulous and made me feel comfortable,” she says. “In my mind, the surgery was not just physical. It was emotional because, to me, they were removing parts of my womanhood. They helped with the education and communication they provided. They came with the care, the uplift, the laughs — all of the things that you need at that time.”
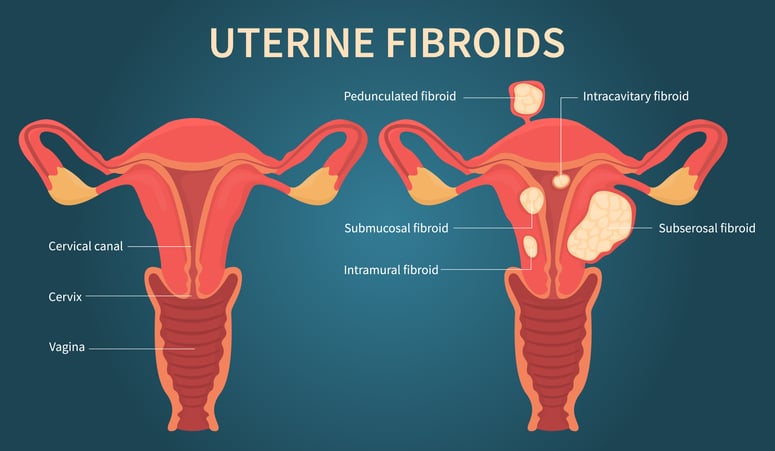
Andrea’s fibroids were inside and outside of her uterus and within the uterine lining, complicating her case.
AT HIGHER RISK
When Andrea’s painful symptoms began two years ago, she initially dismissed them as a natural part of aging – just like other women like her who deal with fibroids.
“Everyone was nonchalant, like, ‘Welcome to being a Black woman over 40,’” she recalls.
But just because an experience is common, Dr. Gray says, doesn’t make it normal. One scientific review found that African-American women have triple the incidence rate and relative risk of fibroids than white women.
“Of the patients I operate on for fibroids, more than 90% are African American,” Dr. Gray says. “Studies have tried to link it to many things, but they have not identified a specific cause.”
The most common symptom of fibroids is heavy menstrual bleeding and longer cycles — Andrea’s longest was 21 days. Other signs are pelvic pain, pelvic pressure, a palpable abdominal mass, constipation, and frequent urination.
“If you are having any of these symptoms, don’t write it off,” Dr. Gray advises.

There are minimally invasive procedures that treat fibroids by blocking their blood supply.
TREATMENT OPTIONS
At first, Andrea wanted to avoid surgery and other invasive treatments, so Dr. Gray prescribed anti-inflammatory medicine to reduce pain and bleeding and suggested lifestyle adjustments.
Andrea tried improving her diet, stretching, and exercising more. For pain relief, she applied heating pads to her abdomen and lower back, took CBD oil, and began spending much more time soaking in the bathtub.
“I couldn’t continue to live like that,” Andrea says. “It’s not conducive to parenting, and my twins were coming up on being high school seniors.”
Fibroid treatments run the gamut from medications and surgical removal to insertion of an intrauterine device that releases progestin, a form of the hormone that plays a role in menstruation. There’s also a minimally invasive procedure known as uterine fibroid embolization that blocks blood flow to the fibroids, Dr. Gray explains.
Andrea also developed anemia, a common side effect of blood loss, and constipation due to fibroids pressing on her bowels. Her symptoms continued to worsen until she decided to undergo a hysterectomy in December 2022.
“I feel better about my decision because Dr. Gray supported the opportunity to explore other options,” Andrea says. “We partnered on what was best for me.”

Andrea says the Methodist Charlton staff lifted her up, calming her fears and making her laugh when she needed it.
OPTING FOR SURGERY
While Methodist Charlton offers robotics-assisted surgeries for many patients, Andrea’s condition turned out to be more complex.
She had three types of fibroids — inside and outside the uterus and within the uterine lining — and some had adhered to her abdominal wall as well as to her bladder, Dr. Gray explains. Her uterus, which typically weighs about two ounces, had swollen to nearly two pounds.
But Dr. Gray and her team were up to the task, even if they had to take a more traditional surgical approach to remove Andrea’s uterus. Afterward, Andrea only had words of praise for the result.
“I had anxiety and fear about the procedure and the outcome. The hospitality of all of the staff helped soothe my fears,” she says. “From the moment the double doors opened, there was a smiling face to greet me and my family when we arrived early in the morning.”
Dr. Gray says she hopes Andrea’s story helps inspire other women struggling with the same thing.
“Listen to your body and go in to be evaluated,” Dr. Gray says. “There are lots of treatments for fibroids. Don’t be afraid that a hysterectomy is your only option.”






