There are a few spare parts that we’re born with but can live without, the tonsils, spleen, and appendix, to name a few. But one organ causes more trouble than it’s worth for millions of Americans.
“If gallstones are a problem, we take care of the troublemaker and remove the gallbladder,” says Joshua Kong, MD, hepatobiliary surgeon on the medical staff at Methodist Richardson Medical Center. “It’s the most common surgery in America.”
It’s estimated that 1.2 million gallbladders are removed each year in the U.S. And about 1 in 5 American adults have gallstones, though many may not know it.
“Not everyone has symptoms,” Dr. Kong says. “But when a gallstone blocks a bile duct, it can cause pain and infection.”
Dr. Kong has performed his share of minimally invasive cholecystectomies, and he discussed the surgery with Methodist Generations, an education and enrichment program for older adults.

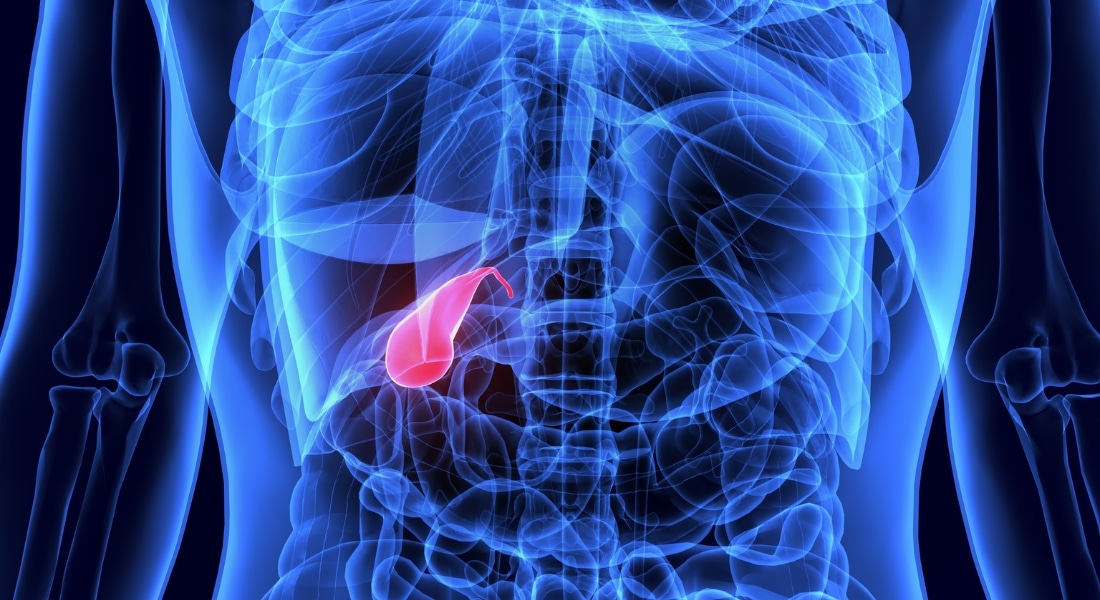
GALLBLADDER DISEASE
The gallbladder is a small pear-shaped pouch that stores bile produced in the liver, releasing it into the small intestine to help us digest fatty foods.
It’s possible to live a healthy life without a gallbladder, and the downsides of removing it are usually less serious than risking future complications by keeping it intact.
“The standard of care when dealing with gallbladder disease is to remove the gallbladder,” Dr. Kong says.
There are a few conditions that require a cholecystectomy, the technical term for this surgery:
- Gallbladder cancer: A rare form of cancer that is most common in patients who suffer with chronic gallstones and inflammation of the gallbladder.
- Chronic cholecystitis: An inflamed gallbladder can be caused by gallstones (calculous) or by bacterial infections or functional diseases (acalculous).
- Gallstone disease: The most common reason for a cholecystectomy. Removing the gallbladder is more effective than breaking up the gallstone, like a kidney stone.
“Patients ask why can’t we just blast the stones with a laser and let them pass like sand?’” Dr. Kong says. “The problem is they’ve tried it, but when the gallbladder is still there, it will continue to make stones. A few months down the road it will come back.”

GALLSTONE SYMPTOMS
Gallstones form when bile inside the gallbladder gets concentrated and sticks together, forming clumps that clog the gallbladder or bile ducts.
“These stones are usually made out of cholesterol, calcium, and bile,” Dr. Kong says. “Some gallstones can get quite big. I’ve seen some that are as big as an apple.”
Gallstones don’t cause problems for most people; it’s when they block a bile duct that they trigger the following symptoms:
- nausea
- abdominal pain, especially after fatty meals
- jaundice, a yellow tint to the skin and eyes
- fever and chills
- elevated heart rate
Gallstones are usually diagnosed with an imaging test such as an abdominal ultrasound, but in some case, further testing is necessary.

HOW SURGERY WORKS
Gallbladder removal is a minimally invasive surgery, with about 90% of cholecystectomies now performed laparoscopically or even with the assistance of a surgical robot.
During the procedure, a surgeon will make one incision near the belly button to insert the laparoscope, as well as two “keyhole” incisions, one to inflate the abdomen with gas and another to insert surgical tools and remove the gallbladder.
“The size of the incision is based on the gallstone size,” Dr. Kong says. “So if you happen to be that person with the apple-size gallstone, then you’ll have a bigger incision.”
The outpatient surgery usually last only 60 to 90 minutes, and the patient goes home the same day. Recovery is fairly quick, and the pain relief can be immediate.
“When I do these surgeries in a healthy patient,” Dr. Kong says, “they usually tell me that the pain that they came in with is gone right away.”
As for side effects, some patients report diarrhea for two weeks after the surgery while their bodies adjust to not having a gallbladder.
“Usually the body will compensate without the extra bile that you store by producing more juice from the liver,” Dr. Kong says. “Some patients need extra help with medication, but after two to six weeks, they don’t need it anymore.”