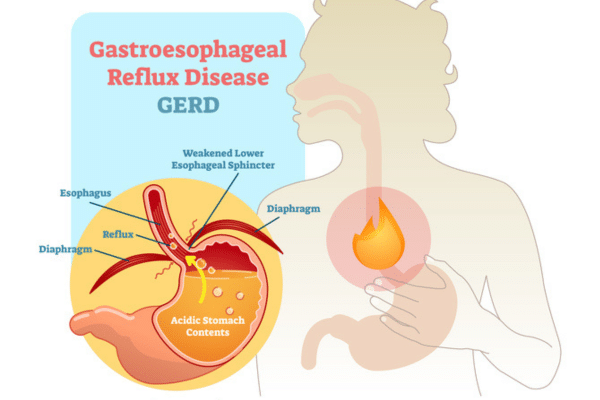
Gastroesophageal reflux disease, or GERD for short, is far more than run-of-the-mill indigestion or acid reflux — a painful reality for 60 million American adults, or about 20% of the population.
“When people think about GERD, they often think it’s just heartburn or some reflux issue,” says Michael Schwartz, DO, gastroenterologist on the medical staff at Methodist Midlothian Medical Center. “There are a lot of different symptoms that come with it.”
Besides heartburn, GERD can cause chest pain, gum disease, sore throat, coughing, and shortness of breath. You can even lose your voice, a condition known as “silent reflux” or laryngopharyngeal reflux (LPR).
“The acid coming up your esophagus can spill into your airway and affect your vocal cords,” Dr. Schwartz says. “So when someone says they have GERD, it just doesn’t mean one thing.”
Dr. Schwartz discussed common misconceptions about GERD, how it’s diagnosed, and how it’s treated during a presentation for Methodist Generations, an education and enrichment program for older adults.
HOW IT’S DIAGNOSED
When patients experience heartburn several times a week and see no improvement with over-the-counter medications, that’s usually when it’s time to visit a gastroenterologist.
“Since symptoms and risk factors for GERD vary by patient, there’s no single lab test that can diagnose it,” Dr. Schwartz says. “The patient’s symptoms guide the route for diagnosis and treatment.”
Dr. Schwartz says there are three primary ways to diagnose GERD:
- Upper endoscopy — This procedure involves inserting a thin, flexible tube with a light and camera through the mouth, down the esophagus, and into the stomach and upper small intestine. The doctor can view the internal lining, check for inflammation or ulcers, and even perform biopsies if needed. During the exam, doctors also measure the acidity (pH) of the reflux to determine how it relates to the patient’s symptoms.
- Bravo test — The Bravo test uses a small, capsule-sized pH sensor attached to the esophagus that wirelessly transmits data to a receiver worn on your belt for 48 to 96 hours. Patients record their meals and symptoms to help doctors connect acid levels with discomfort. The capsule naturally detaches and passes through the body after the test.
- Drug trials — Some patients may participate in clinical trials where they take an investigational drug or placebo, track their symptoms, and undergo monitoring procedures. These trials help researchers evaluate the safety and effectiveness of new treatments.
Trust your gut to advanced GI care at Methodist by finding a digestive health specialist near you. Visit MethodistHealthSystem.org
Left untreated, GERD can lead to serious complications like inflammation or ulcers in the esophagus, scarring that makes swallowing difficult, asthma, and even periodontal disease — inflammation of the gums caused by regurgitated stomach acid.
Dr. Schwartz uses a football metaphor to explain how patients and doctors can work together to combat GERD.
“Your defense is watching your portion sizes and being mindful of your eating position,” he says. “Don’t eat and then go to bed. Sitting nice and upright allows gravity to aid in the digestive process.”
When it comes to offense, there are a host of treatments from natural remedies to the “latest and greatest” medications, as well as surgical options when those don’t work.

OFFENSE: TREATING GERD
For mild acid reflux, gastroenterologists often recommend starting with simple, natural remedies. Common household treatments like aloe, baking soda mixed with water, or apple cider vinegar may temporarily relieve symptoms but aren’t long-term solutions.
If that doesn’t work, medications may be prescribed. One newer option, potassium-competitive acid blockers (PCABs), works almost instantly compared to traditional drugs that take hours to become effective.
“The medications we’re using today are the latest and greatest,” Dr. Schwartz says. “They represent the future of reflux treatment.”
For more severe cases, a surgical procedure known as Nissen fundoplication may be considered. However, surgery is not a cure-all and comes with potential complications.
“Gastroenterologists are generally cautious about recommending surgery,” Dr. Schwartz notes. “There’s no reason to undergo a major surgery when GERD can be managed with medication. In fact, about 40% of patients who have surgery end up back on medication within five years.”

DEFENSE: PREVENTING GERD
Preventing GERD often comes down to everyday habits. Doctors recommend sitting upright during and after meals to use gravity to help keep food in the stomach and waiting at least a couple of hours before lying down or going to bed.
“Keeping meal portions moderate and low in fat can make a big difference,” says Dr. Schwartz. “It’s also important to be cautious with over-the-counter medications commonly used to relieve arthritis, joint pain, and headaches.”
This is because regular or high-dose NSAIDs like ibuprofen (Advil) can bother the GI system, leaving the stomach and intestinal lining vulnerable to damage from stomach acid.
Simple lifestyle changes such as maintaining a healthy weight, reducing stress, staying hydrated, and avoiding trigger foods can also go a long way toward supporting digestive health.