Retired accountant Steve Peacock knew he was due for a chest exam when a CT scan found a suspicious nodule that turned out to be lung cancer.
It was the swift chain reaction that discovery triggered that surprised Steve, from a minimally invasive ION biopsy days later to lung surgery the following month at Methodist Dallas Medical Center.
“It was lightning speed,” he says. “They were very professional and very fast.”
A year after his surgery, Steve is back to “puttering around” his Waxahachie farm, cancer-free and grateful that he sought out lifesaving care when he did. What’s more, he hopes others will follow his lead.
“Maybe they smoked, or they’re just due for a checkup,” he says. “Make sure your lungs are in good condition because that’s the deadliest form of cancer.”

SCREENING SAVES LIVES
Lung cancer claims 125,000 lives each year, more than colon, breast, and prostate cancer combined.
The fact that symptoms often go unnoticed because there are no pain receptors in the lungs makes screening critical, especially for longtime smokers like Steve.
What distinguished his case, however, was the pain. It was excruciating enough at times that it caused Steve to double over.
“I thought it was a heart attack, where it was tremendously painful for a short period of time, and then the pain would go away,” he says.
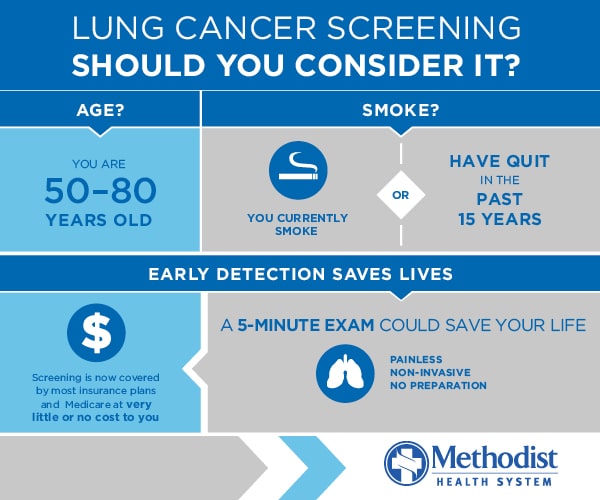
That pain inspired him to seek out a noninvasive CT scan, recommended for anyone 50 to 80 years old who is a current smoker or kicked the habit within the past 15 years.
“Twenty-five years ago, there was no screening for early-stage cancer like Steve’s,” says Jagadeshwar Reddy, MD, a pulmonologist on the medical staff at Methodist Dallas. “Now we find these nodules a lot sooner, before the cancer can progress.”
ION CHANGES BIOPSIES
Another recent advance in lung cancer treatment involves how doctors collect biopsies to determine whether a mass is cancerous.
“The old way involved putting a patient in a scanner and inserting a needle into the chest,” Dr. Reddy says. “The problem is that many of these patients are former smokers struggling with emphysema, and the chance of a collapsed lung could be as high as 25%.”
The Ion platform reduces that risk to below 1% because it accesses the airways using a flexible catheter that’s inserted through the nose or mouth while the patient sleeps.
Developed by Intuitive, the same company behind the da Vinci Surgical System, Ion creates a turn-by-turn path to the nodule, even in hard-to-reach parts of the lung.
“More than 90% of the time, if there’s cancer we are able to find it,” Dr. Reddy says. “And we don’t risk a lung collapse that may require a chest tube and days in the hospital.”

‘WE CARE ABOUT THEM’
Steve’s biopsy in November 2024 determined that his nodule was cancer, and he was quickly referred for surgery with David Mason, MD, a thoracic surgeon on the medical staff at Methodist Dallas.
“A case like Steve’s really highlights how well we work as a team,” he says. “We pride ourselves on our speed and communication. Every one of my patients has my cell number.”
Cancer won’t wait if someone “drops a ball,” Dr. Mason adds, and no patient with cancer should have to wait any longer than absolutely necessary to address a life-threatening diagnosis.
That’s why Steve’s resection surgery proceeded shortly after his biopsy. He spent a few days at Methodist Dallas and underwent chemotherapy after that. A follow-up scan a year later came up clear, but that doesn’t mean he’s heard the last of his doctors.
“These are our patients for life,” Dr. Mason says. “I have patients who are 10 years out from surgery that I continue to follow. We care about them.”
That level of care wasn’t lost on Steve, who acknowledged his caregivers “spent more time with me than I thought doctors spent with patients these days.” And he’s grateful for every minute.
“I have a debt to pay to Dr. Mason, Dr. Reddy, and their entire teams,” Steve says. “The care they gave me is something I will remember for the rest of my life.”






