Crohn’s disease, a painful and chronic form of inflammatory bowel disease (IBD), is becoming increasingly common, especially among younger adults. Despite greater awareness, many cases still go undiagnosed until complications arise later in life.
“I’ve seen a noticeable increase in Crohn’s cases over the past decade, particularly in patients in their 20s and 30s, as well as others being diagnosed much later than ideal,” says Muhammad Baig, MD, a gastroenterologist on the medical staff at Methodist Dallas Medical Center. “Starting treatment early significantly reduces the risk of complications.”
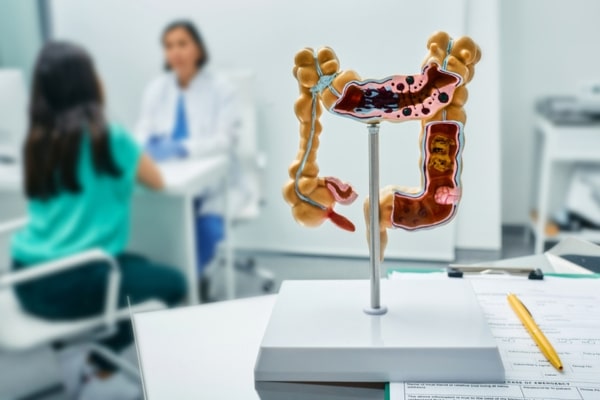
Crohn’s disease affects around 750,000 Americans and can present in very different ways. Some patients experience constipation, while others deal with persistent diarrhea.
“It’s an inflammatory condition that can affect any part of the gastrointestinal tract,” Dr. Baig explains, “from the mouth all the way to the rectum.”
Common symptoms include abdominal pain, fatigue, weight loss, and blood in the stool. In some cases, symptoms appear outside the digestive system in skin rashes, mouth ulcers, or hair loss.
While Crohn’s has no cure, its symptoms can be controlled through medical management.
The exact cause of Crohn’s is unknown, but certain patients are at increased risk.
RISK FACTORS
The root cause of Crohn’s remains unclear, but it is linked to a malfunction in the immune system.
Several factors may increase a person’s risk:
- Family history: Up to 20% of people with IBD have a first-degree relative who also has Crohn’s or ulcerative colitis.
- Age and ethnicity: Crohn’s is often diagnosed in teens or young adults, and is more prevalent among individuals of Eastern European descent.
- Environmental factors: Living in urban or industrialized areas may also elevate risk compared to rural or less developed regions.
GI specialists have a number of tools at their disposal to diagnose and treat Crohn’s disease.
HOW IT’S DIAGNOSED
For younger adults experiencing ongoing gut health issues, a gastroenterologist can use various tools to investigate, including imaging studies, lab tests, and colonoscopy.
“Our diagnostic capabilities have improved a lot,” Dr. Baig says. “We now have better blood and stool tests, along with endoscopic procedures, to accurately diagnose Crohn’s.”
Early detection is key because long-standing inflammation can lead to irreversible damage to the digestive system.
“A lot of people think colonoscopies are only needed at age 45 for cancer screening,” Dr. Baig says. “That’s true only for people without symptoms. If you have issues, you shouldn’t wait.”
Untreated Crohn’s disease can lead to intestinal blockages caused by scarring, sometimes requiring surgery to remove part of the bowel. In severe cases, patients may need a temporary or permanent ostomy bag.
“Delaying diagnosis increases the chances of needing surgery and losing part of the intestine,” Dr. Baig warns. “Catching it early can prevent major complications.”
Crohn’s also increases the risk of colon cancer, reinforcing the need for timely evaluation.

Keeping a food diary may help fend off flare-ups by avoiding problem foods.
MANAGING FLARE-UPS
Treatment options for Crohn’s have expanded significantly in recent years. New oral medications, injections, and infusions offer better control — even for hard-to-treat cases.
“These treatments are much more effective when the inflammation is caught early,” Dr. Baig says. “Once scar tissue forms, medications aren’t as helpful.”
With the right treatment, Crohn’s can enter remission, with symptoms subsiding or disappearing. However, flare-ups can still occur, often triggered by diet or stress.
Dr. Baig advises patients to simplify their diets during flare-ups:
“Stick to bland, single-ingredient foods and avoid processed or packaged foods,” he advises.
Dr. Baig also emphasizes the role of stress: “Daily stress reduction is essential for maintaining gut health.”
Regarding gluten, Dr. Baig notes that while celiac disease sometimes co-exists with Crohn’s, not all patients need to avoid gluten.
“I screen all Crohn’s patients for celiac,” he says, “but I don’t impose unnecessary dietary restrictions.”
Flare-ups are a signal that something may be off, Dr. Baig says.
“If you notice symptoms like bleeding, altered bowel habits or unusual pain, your treatment may need to be adjusted,” he says. “Don’t wait — consult a gastroenterologist and get evaluated early.”