If not for her dog Bandit, Wendy Aschner suspects she might not have woken up when blood clots took her breath away and led to a lifesaving visit to Methodist Richardson Medical Center.
For weeks after her second hip replacement, the 74-year-old Richardson resident had been feeling exhausted, as though she couldn’t take a full breath. Then one night last fall, her beloved Bernedoodle came to the rescue, waking her up at 5 a.m. to go outside.
“I had no breath,” she says, recounting collapsing back into bed after letting Bandit back inside. “My husband, he said, ‘What’s wrong?’” All I could get out was, ‘Call paramedics.’”
Wendy had a massive pulmonary embolism — stretching across most of her right lung and into her left — that would need to be removed by Mohamad Kabach, MD, interventional cardiologist on the medical staff at Methodist Richardson.
“It was very frightening,” she says. “But Dr. Kabach and his team were so kind and reassuring. He’s my hero.”

Wendy had both hips replaced and developed deep vein thrombosis while recovering from the second surgery.
BOTH HIPS REPLACED
Blood clots are a possible complication for patients who undergo surgeries that leave them immobile, Dr. Kabach says.
But Wendy’s case was somewhat unusual. After her first hip replacement in March 2022, Wendy was diligent about going to rehabilitation sessions, wearing her compression socks, and taking her medication.
She experienced no complications and felt comfortable with the second hip replacement last August. Neither of those surgeries were performed at Methodist Richardson.
Days after the second replacement, Wendy went to rehab and said she suspected something was wrong because she was so exhausted. Three weeks later, she developed a cough, which she thought was bronchitis.
“It just got worse,” Wendy says. “I knew there was something wrong, but I couldn’t put my finger on it.”
No one could until the morning she met Dr. Kabach and his team at Methodist Richardson in October 2023.

A CT scan revealed the pulmonary embolism that was disrupting the blood flow in Wendy’s lungs.
BLOOD CLOTS IN THE LUNGS
Before dawn that morning, paramedics rushed Wendy to the hospital’s emergency department, where the medical team conducted tests to determine why she couldn’t breathe.
Dr. Kabach took a look at her scans and quickly determined that Wendy needed to go to surgery immediately because large blood clots had formed on both sides of her lungs.
Having such a large embolism in the lungs can make it difficult to breathe, and it is often life-threatening. In most cases, they can be treated with anti-coagulant medications that dissolve the clots, but when they are as large as Wendy’s, surgery may be necessary.
Pulmonary embolisms are common, ranking just below heart attacks and strokes among cardiovascular diseases, and affect up to 900,000 people in the U.S. every year, according to the American Lung Association.
Wendy was quickly taken into an operating room, where the clots were removed from her lungs using a catheter and a minimally invasive procedure known as a thrombectomy.
“Patients with such a large pulmonary embolism feel suffocated. They feel terrible up until you actually remove the clot,” Dr. Kabach says. “And that’s exactly what happened to Wendy, she had that one perfect moment. I removed one big clot, and she goes, ‘Gosh, now I can breathe.'”
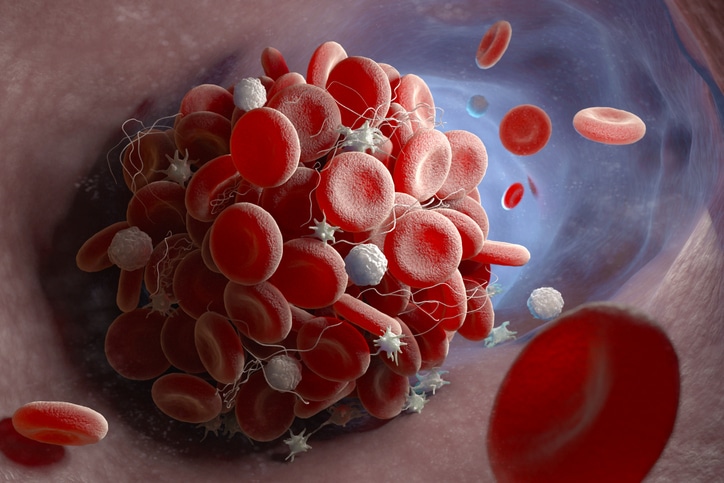
A pulmonary embolism is often caused by a blood clot that forms in the legs, a condition known as DVT.
DEEP VEIN THROMBOSIS
After the procedure, Dr. Kabach determined that Wendy’s embolism stemmed from her hip replacement. Because patients are at higher risk of developing blood clots after surgery on their lower extremities, they are often required to go to rehab and be placed on blood thinners to help prevent clots from forming.
“A pulmonary embolism usually starts from a clot in the lower extremities, a condition we call DVT — deep vein thrombosis,” Dr. Kabach says. “In some cases, that clot can dislodge from the lower extremity vein, travel through the heart, and land in the pulmonary artery.”
Following orthopedic surgery, Dr. Kabach says patients should be on the lookout for swelling, pain, and discoloration in the leg, as well as dizziness, chest pain, and shortness of breath. Fainting or passing out is also a major sign of a pulmonary embolism, he says.
“Passing out is just enough of a story — with recent surgery — to consider a pulmonary embolism,” he says.

Finally cleared to travel after her health scare, Wendy is excited to visit her sisters in her native England.
‘I CAN GO HOME’ TO ENGLAND
For weeks after the clot was removed, Wendy struggled to walk for more than five minutes. But when she finally managed to walk to the stop sign at the end of her street, she knew she could bounce back.
She credits her recovery to Dr. Kabach and his team but also to the encouragement of her family, including her sisters back home in her native England, her husband, their four grandchildren, and Bandit, of course.
“When I was recovering from the embolism, he just laid next to me the whole time,” Wendy says. “He’s just Mummy’s boy.”
At a recent follow-up visit, Dr. Kabach took Wendy off her blood thinners and cleared her for travel. The timing couldn’t be better for Wendy, who will soon travel “across the pond” to see her sisters, one of whom just turned 80.
“I can go home,” says Wendy, who missed the birthday party but plans to make a surprise visit. “I can go home and see my sisters.”






