Colon cancer is the fourth most common cancer in the United States, and it’s estimated that over 150,000 new cases will be diagnosed in 2022, according to the Centers for Disease Control and Prevention.
“Every American is at average risk for colorectal cancer,” says Paul Hackett, MD, colorectal surgeon on the medical staff at Methodist Charlton Medical Center. “There are no low-risk people for colorectal cancer in the U.S. based on the prevalence of this disease.”
But the news isn’t all doom and gloom, he adds. There are steps we can take to protect our health and understand our risk factors.
“Colon cancer is preventable,” Dr. Hackett says. “It is one of those things that can show up in 100 different ways in 100 different people. No concern is too small to check with your doctor about.”
Here are three things everyone should know about colon cancer:

1. MONITOR BATHROOM HABITS
Our bodies have a way of sounding the alarm when something is wrong, and any deviation from your normal pattern should at least raise a red flag.
“Getting screened at the recommended age, 45, is one way to stay proactive,” Dr. Hackett says. “The other is simply turning around and looking in the toilet after every bowel movement. You’ll find what’s normal and be the first to detect anything unusual.”
One of the biggest indicators is bleeding, he explains. It’s also important to note persisting changes in bathroom patterns and stool shape.
“If a person who is regular all of a sudden notices they’re not having bowel movements as frequently as they used to or if their stools become narrow all of the time, it could be the result of a mass in the rectum or lower colon.”
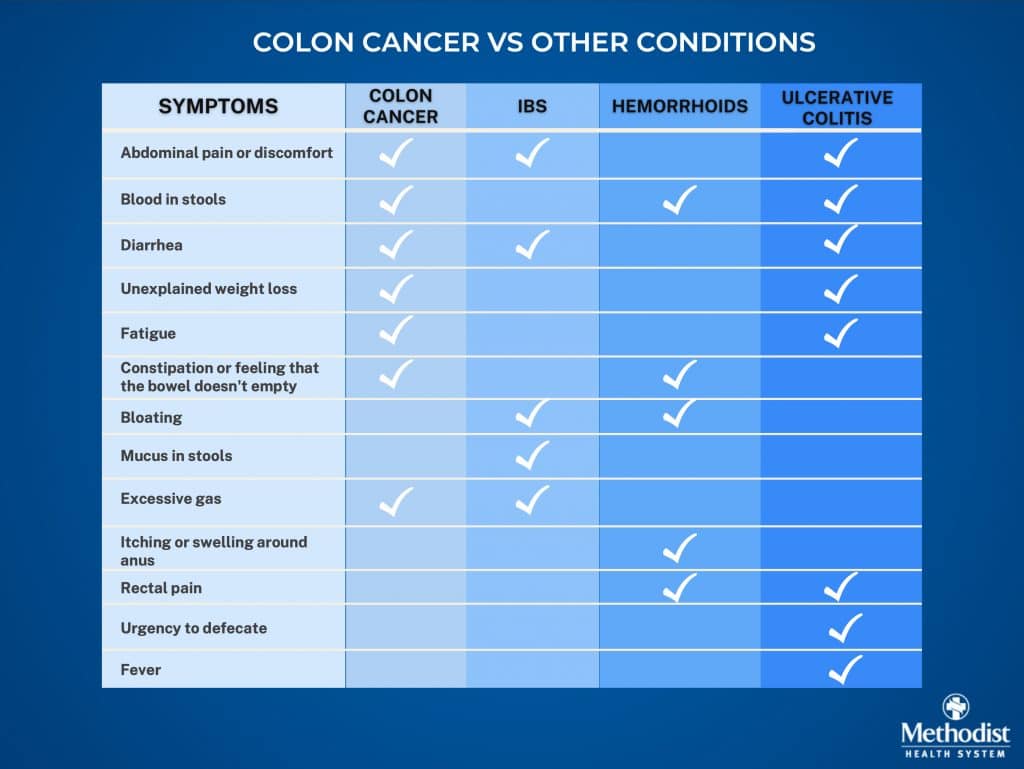
Of course, some symptoms of colorectal cancer can overlap with those of other conditions like irritable bowel syndrome or ulcerative colitis. So telling your doctor about previous medical conditions and your list of medications — some of which may have gastrointestinal side effects — is invaluable when it comes to finding answers.
“About 80% of diagnoses are going to be determined by health history,” Dr. Hackett says. “So we’ll ask about bleeding, if you’re experiencing pain, and the history of your bowel function.”

2. KNOW YOUR FAMILY HISTORY
While researchers cannot pinpoint a cause for colorectal cancer, certain hereditary conditions and lifestyle choices are associated with higher risk, including a family history of polyps, high alcohol consumption, smoking, and a diet high in red meat and low in fiber.
While the recommended age to begin regular screenings is 45, people who are considered high risk should get evaluated years earlier — particularly those with a family history of the disease, Dr. Hackett says.
“For example, if your mother was diagnosed with colon cancer when she was 40,” he explains, “then you should get a colonoscopy 10 years before her age of diagnosis — in this case, 30.”

3. SCREENING SAVES LIVES
Being proactive about your health is key to effective treatment — as proved by this DeSoto woman who felt completely healthy despite her early-stage cancer. She credits her sister’s cancer diagnosis with saving her own life.
Family links are a common theme that emerges in cancer research, Dr. Hackett adds.
“The first thing I want to know about is family history, focusing on immediate relatives — mother, father, children, and siblings,” he says of the initial process. “I’m looking for a history of colon cancer or colon polyps.”
After doctors assess your risk, there are several screening options you may consider. Certain tests require stool samples to look for hidden bleeding — a possible symptom of colon cancer — or abnormal DNA markers that will identify pre-cancerous polyps or colorectal cancer, Dr. Hackett explains.
Take our colon cancer health risk assessment to learn more about your risk. Visit MethodistHealthSystem.org
Doctors can also perform radiographic scans to examine the colon. They require some prep work but can be done without anesthesia, Dr. Hackett explains. The average person should have them done every five years.
But the gold standard of colon cancer screening is a colonoscopy. Not only does it allow physicians to identify potential tumors, but it allows them to remove the tissue for further analysis.
“If your colonoscopy is negative for abnormal results, it should be done every 10 years,” Dr. Hackett says. “If something does come up — depending on the size and type of polyp they find — you should have them done at shorter intervals.”
Because of the high rate of disease, having an open and honest dialogue with your doctor can be lifesaving, Dr. Hackett says.
“You have to take screenings seriously and communicate with your primary care physician if something needs to be investigated further,” he says.

