Varicose veins make life miserable for millions of Americans, and until recently the procedures to treat them could be just as painful.
But new advances have allowed physicians to move beyond ablation, which destroys the veins with heat, or “vein stripping,” a surgery that can be as painful as it sounds.
“For the patient, options like VenaSeal are far more comfortable,” says Anas Alomar, MD, medical director of cardiology and chair of the department of medicine on the medical staff at Methodist Southlake Medical Center. “We don’t do vein stripping anymore because it’s painful, invasive, and has risks.”
Rather than removing or destroying varicose veins, VenaSeal closes off weakened veins using medical adhesive, allowing the body to naturally absorb them and divert the blood they carry. Methodist Southlake recently treated its first VenaSeal case.
“It’s an outpatient experience,” Dr. Alomar says. “People walk out of the procedure room on their own.”
HOW DO VARICOSE VEINS FORM?
Any vein close to the skin’s surface can become a varicose vein, but these enlarged and twisted blue or purplish veins are most commonly found in the legs.
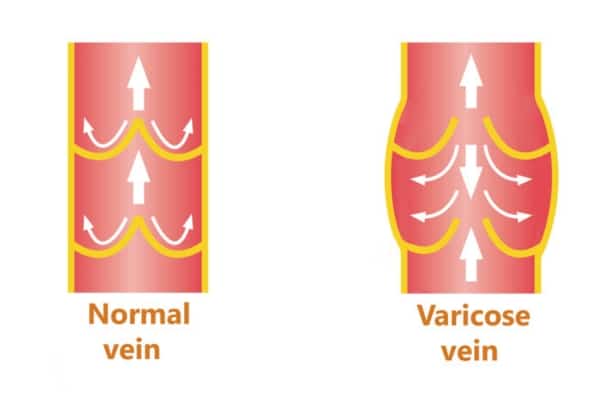
Blame gravity for the damage that causes varicose veins. In a healthy vein, tiny valves push the blood from the lower extremities to return blood to the heart. That blood can pool in damaged veins, which have been weakened by the wear and tear of age, pregnancy, or obesity, or simply because of genetics.
While often a cosmetic concern, Dr. Alomar says, varicose veins can also cause painful symptoms, from heaviness and cramping to numbness and swelling — and in the worst cases, skin ulcers and blood clots.
“Those ulcers can get infected and cause a lot of problems,” he says.

HOW DOES VENASEAL WORK?
Like ablation, VenaSeal seals off damaged veins, but it uses medical-grade adhesive rather than radiofrequency heat.
“Ablation requires multiple injections of the legs,” Dr. Alomar says, “and it can have side effects, like burn injury to the skin.”
In contrast, sealing up varicose veins using VenaSeal is minimally invasive, causes no discomfort, and allows for a much faster recovery time.
A catheter is used to deliver the adhesive, which holds the walls of the vein together. That redirects the blood flow to healthier veins, effectively eliminating the varicose veins.
Those unused veins are eventually absorbed by the body because there’s an abundance of other veins in the lower extremities to pick up the slack.
“Most people think about how bad it is to block arteries because that is limiting the blood flow going to the foot,” Dr. Alomar says. “Veins are more forgiving because there are more of them in the legs.”

WHAT ARE THE BENEFITS?
Perhaps the biggest benefit of solutions like VenaSeal is how quickly patients see improvement.
“Patients should be able to see results from the treatment almost immediately. The treated veins will start to fade, and any pain or discomfort should begin to improve,” Dr. Alomar says. “In most cases, the results are permanent, and patients will not need any further treatment.”
That’s not to say VenaSeal is for everyone. Before the procedure is approved, a screening process will ensure patients are viable candidates to undergo the treatment. This process features a series of ultrasounds so providers can look at the veins and find what issues are happening inside the legs.
“We confirm that patients have venous insufficiency, confirm that the veins are big, and talk to them about a potential allergy to the glue,” Dr. Alomar says.
While some patients may suffer from inflammation or an allergic reaction to the glue, the five-year success rate for VenaSeal is nearly 95%. Other benefits include:
- No discomfort and less bruising
- No need for tumescent anesthesia injections
- Faster recovery time than thermal ablation
Indeed, the recovery is quick enough that Dr. Alomar recommends patients return to their usual routine the very same day. No compression stockings or downtime are necessary.
“We recommend patients be active on the day of the procedure so they can walk and resume normal activity,” he says.






