The aging process may be most obvious in gray hair and sagging skin, but vital organs age, too, and good health is most vulnerable to changes that aren’t skin deep.
As our hearts age, they become more susceptible to disease. Arteries harden and narrow, high cholesterol gums up blood flow, valves calcify, and the electrical system keeping the heart in rhythm misfires. Worst of all, parts of the heart can simply cease to function.
”After a heart attack, part of the heart muscle can die, and the heart can change its shape,“ says Mihaela Kruger, MD, interventional cardiologist on the medical staff at Methodist Southlake Medical Center. ”As the heart muscle becomes larger and weaker, pressure builds inside the heart and leads to fluid buildup in the lungs, causing congestive heart failure.”
Dr. Kruger sat down with a group from Methodist Generations to talk about all the ways our hearts age and share some suggestions about how to turn back the clock.
From prevention to advanced procedures, trust your heart to the innovative, personalized care that Methodist provides. Visit MethodistHealthSystem.org
HARDEST WORKING MUSCLE
Like other muscles in our bodies, the heart muscle can grow and thicken, especially if it’s working harder than it should be, even at rest.
“In people who have high blood pressure for a very long time, it‘s as if the heart is lifting weights,” Dr. Kruger says. “The left ventricle works hard to overcome the high arterial blood pressure. So the heart muscle gets thicker.”
But unlike our biceps and quadriceps, a thicker heart doesn’t function nearly as efficiently because the arteries that supply it don’t grow with it. A thicker heart muscle also becomes stiff and can’t relax as well.
This leads to diastolic congestive heart failure, when the pressure builds up in the hear and then backward in the lung circulation, causing shortness of breath and fluid buildup.

ELECTRICAL SYSTEM
Believe it or not, the human heart has more in common with an EV than an internal combustion engine — because it runs on electrical impulses.
Each heartbeat is driven by the sinus node, a small mass of tissue that sends out 60 to 100 electrical pulses per minute. But sometimes, with the wear and tear of age, that natural pacemaker gets out of sync.
“The electrical system of the heart can change with age,” Dr. Kruger says. “When people complain of heart palpitations, they may feel dizzy or like they‘re going to pass out. They can mistake fast heart rates for anxiety.”
An abnormal heartbeat, or arrhythmia, occurs when disease slows down the sinus node or when another part of the heart becomes electrically active and takes over and misfires. Considering the heart beats 35 million times a year, it’s no wonder it can lose a step after decades of nonstop exertion.
“There’s ongoing wear and tear of the electrical system, just like any other parts of our bodies,” Dr. Kruger says. “And this is the reason that electrical system degenerates.”
Arrhythmias can run in families, but chronic diseases like diabetes and lifestyle factors also play a role, including smoking and overindulging in alcohol and caffeine.
GET THE BLOOD PUMPING
The heart may run on electrical impulses, but it’s also a kind of hydraulic system, and blood is the fluid that fuels that pump.
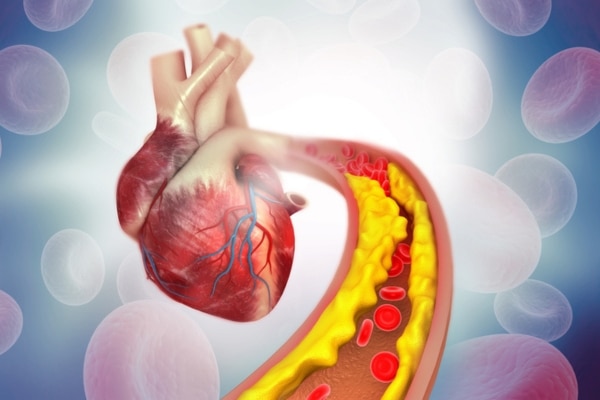
As we age, the blood supply can become less reliable because of coronary artery disease, which causes the arteries that carry the blood to harden and narrow. Fatty deposits known as plaques can build up inside them and block the flow partially or completely.
When these plaque deposits crack and erode, what’s inside gets exposed to the bloodstream, causing the sticky cells in the blood, the platelets, to form blood clots and shut down the blood flow. That disrupted blood flow robs the heart of its oxygen supply, causing muscle cells to die and weakening the organ.
“Heart attacks happen when that plaque becomes unstable and causes a blockage, even when the blockage is not very severe,” Dr. Kruger says. “It can be a 30% or 40% narrowing of a blood vessel that under the right circumstance can become unstable.”
A more severe narrowing, of 80% or 90% can cause chest pain or angina, and is a common reason for patients to receive heart vessel stents or in severe cases, coronary artery bypass.
WHEN HEART VALVES FAIL
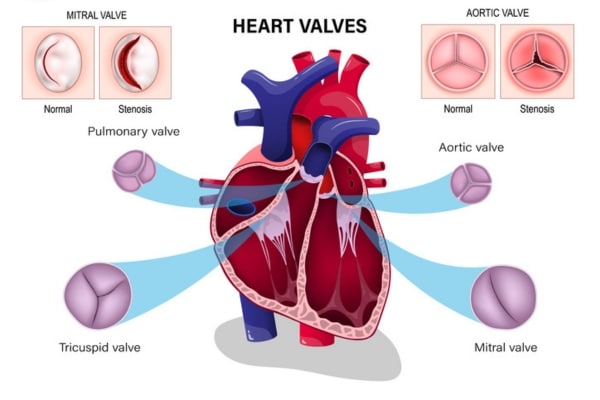
While keeping arteries healthy is critical to deliver blood to the heart, the flow of blood through the heart relies on a series of four valves, each of which consists of small flaps of tissue, or leaflets, that open and close with each heartbeat.
“Over the course of a lifetime, after opening and closing millions and millions of times, these valves can get damaged,” Dr. Kruger says. “They can weaken or start to leak with decades of wear and tear.”
A patient with heart valve disease might suffer from a number of different problems:
- Stenosis — When the leaflets stiffen, the valve narrows and reduces the amount of blood flowing through the heart.
- Prolapse — If the leaflets in the mitral valve are too stretchy, a patient may suffer from mitral valve prolapse (MVP), where the leaflet flops back into the left ventricle and allows blood to flow backward.
- Regurgitation — If the leaflets fail to seal completely with each heartbeat, blood can leak backward through the valve, forcing the heart to work harder to compensate.
Doctors often detect heart valve disease when they hear a heart murmur while listening to a patient’s heartbeat with a stethoscope.
“When your doctor says that you have a heart murmur,” Dr. Kruger says, “that‘s because we hear the blood flow going through the heart valves.”
Most heart murmurs are harmless, or “innocent,” and don’t cause other symptoms, but when a heart murmur is accompanied by chest pain or shortness of breath, it’s time to see a doctor.

TURNING BACK THE CLOCK
Not all chronic diseases are reversible, but heart disease in its early stages can be corrected with some simple lifestyle changes, whether it‘s watching what we eat, being more active, cutting down on alcohol, or kicking the worst habit of all.
“It’s never too late to stop smoking,” Dr. Kruger says. “Even if you have smoked for many, many years and are in your 60s or 70s, stopping today is still a lot better than continuing.”
Becoming more conscious of our diets is also an important step in taking care of an aging heart, especially cutting out saturated fats, sugars, and salt.
“It’s really critical to keep your sodium intake down,” Dr. Kruger says. “Too much sodium causes our bodies to retain water, and that in turn leads to high blood pressure.”
Finally, stress can have a major negative impact on your heart health because it increases cortisol and adrenaline, raising your heart rate and blood pressure.
“We need to learn how to destress for our hearts‘ sake. Easy to say, hard to do,” Dr. Kruger said. “But meditation, practicing mindfulness, and exercising daily — they all can help.”
Dr. Kruger suggests staying active, not just for the usual reasons, but also so that changes in our hearts don’t catch us by surprise after the damage has been done.
“If we stay active, not only do we prevent some of the heart problems, but we may notice symptoms of heart disease before they become severe enough to catch us by surprise, at rest,” she says.
After all, the heart is the hardest working organ in our bodies, pumping 2,000 gallons of blood every day and beating 2.5 billion times by the time we’re 70. It only makes sense to do everything we can to stay young at heart.






