Working or exercising in triple-digit temperatures can quickly become dangerous, even for the heartiest roofer or the fittest runner. That’s because there’s a limit to how much extreme heat our bodies can beat.
“Athletes and workers will try to tough it out because they think they’re better equipped to deal with the heat,” says Benjamin Lo, MD, medical director of the emergency department at Methodist Midlothian Medical Center. “But they’re the ones who come into the ER really sick.”
Heat illnesses are on the rise in Dallas-Fort Worth, with hundreds of cases serious enough to be reported. Blame the humidity, like the old saying goes, because when it gets muggy and hot, not only does it feel hotter (what’s called the heat index) but our bodies have a harder time cooling down by sweating.
“When the humidity approaches 75% and above, the body can only sweat so much and then it’s just too humid to cool down effectively,” Dr. Lo says.
But how do you stay safe when heat indexes are routinely above 110? What are the warning signs you’re overheating? And how can you avoid a trip to the ER? Dr. Lo has some advice.

WHO’S AT RISK?
Dr. Lo is quick to emphasize that no one is immune to heat illness, regardless of your fitness level or how acclimated you are to the heat.
“A lot of people think if they’re in really good shape, they can handle the heat. And that’s not really true at all,” he says. “Most people’s bodies regulate the heat the same whether you have good exercise tolerance or not.”
Most of us understand that we sweat to cool down, but the key step in that cooling process is evaporation. When the air is humid, it’s already saturated with water. If our sweat can’t dissipate heat into the air, our bodies can’t cool down as efficiently.
Older adults and young children are among the most vulnerable to heat because their bodies don’t adapt to extreme temperatures as well. In the case of seniors, their blood vessels don’t dilate as easily, and they lose the ability to sweat as much.
“Families may take Grandma on a walk for five or 10 minutes at most,” Dr. Lo says, “and they’re coming into the ER for heat exhaustion or even heatstroke.”
Another at-risk population includes patients who use diuretic medications to treat high blood pressure, as well as heart, liver, and kidney disease. Also known as “water pills,” these drugs pull water out of the body by promoting urination.
“People who take these medications are kind of almost already dehydrated,” Dr. Lo says. “Even younger people in their 40s and 50s who take these medications can go outside and get overheated within just 20 or 30 minutes.”
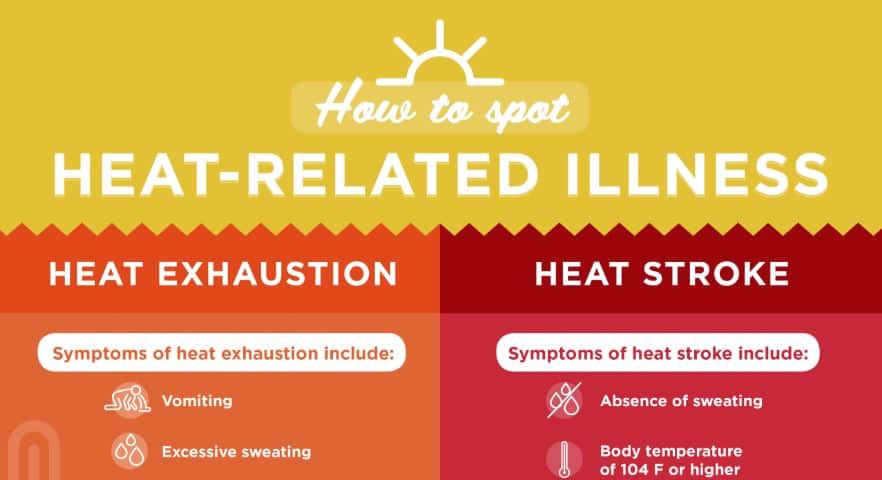
Click on the graphic above to learn more about how heat exhaustion and heatstroke differ.
SIGNS YOU’RE TOO HOT
Heat illnesses can escalate rapidly from a prickly heat rash to exhaustion to heatstroke if you spend too much time outdoors in the Texas heat.
The first dangerous stage is heat exhaustion, which often begins with muscle cramps before a range of other symptoms set in.
“People will sweat a lot, they’ll get a headache, they’ll get dizzy,” Dr. Lo says. “Sometimes they can get nauseous or feel like they’re going to faint.”
Patients with heat exhaustion typically still have a normal body temperature, although their pulse might quicken and they may breathe faster. Get them out of the heat quickly, even if it’s just into the shade. Cool them off to avoid the next stage: heatstroke.
“Heat exhaustion may not require a trip to the hospital but should be rapidly treated with wet rags and hydration,” Dr. Lo says. “Heatstroke is an emergency and requires immediate medical attention.”

DON’T WAIT TO GET HELP
When heatstroke sets in, the body has lost its ability to cool down on its own. Patients often stop sweating and their body temperature rises. One of the key signs is impaired mental acuity.
“A lot of these patients will become very, very confused,” Dr. Lo says. “Some of them will be unresponsive when we find them.”
In these situations, play it safe and call for help immediately. Paramedics and ER staff can stabilize heatstroke patients with ice packs and cooling fluids with electrolytes delivered intravenously. They may even insert tubes into the chest to pump fluid into the cavity around the lungs.
“In most cases, ice works really well,” Dr. Lo says. “That, plus IV fluids, is usually the only thing patients really need.”
The key to avoiding a trip to the hospital is to recognize the early signs of heat exhaustion and to stay hydrated, preferably with fluids containing electrolytes and not sodas or high-caffeine sports drinks that are diuretics, too. But first and foremost, get out of the heat.
“The mistake many people make is to leave an overheated patient in the heat and bring things to them,” Dr. Lo says. “At a soccer game, for example, they’ll bring a wet rag or a cold drink to that patient when the important thing is to remove them from the heat first.”






