Summer heat can be dangerous for anyone, but older adults are especially vulnerable because their natural cooling systems don’t function as well as they used to.
Maybe they don’t sweat enough, or they suffer from poor circulation — biological changes that occur to everyone as we age. But older adults may also struggle with diseases that make them more susceptible to the heat or take medications that raise their risk of overheating.
“It’s the perfect setup for body temperature to go up and up,” says Robert Simonson, DO, chair of emergency medicine at Methodist Dallas Medical Center.
In general, Dr. Simonson suggests that anyone 62 or older who is overheated and has signs of heat exhaustion head straight to the emergency room. Here, he shares some warning signs and ways to help us all cope with the heat this summer.

STAGES OF HEAT ILLNESS
Older adults may not realize when the heat is too much for them, Dr. Simonson says.
For example, heat indexes in the 90s may be uncomfortable for young and old alike, but that temperature could be deadly for a grandmother cooped up in an apartment during a power failure.
Heat cramps, the first stage of heat illness, manifest with fatigue, thirst, and muscle cramps. The body temperature itself may be normal.
A patient with those symptoms could succumb to the heat if they can’t cool off by first getting out of the heat and into an air-conditioned space and then rehydrating with water or electrolyte solutions like sports drinks.
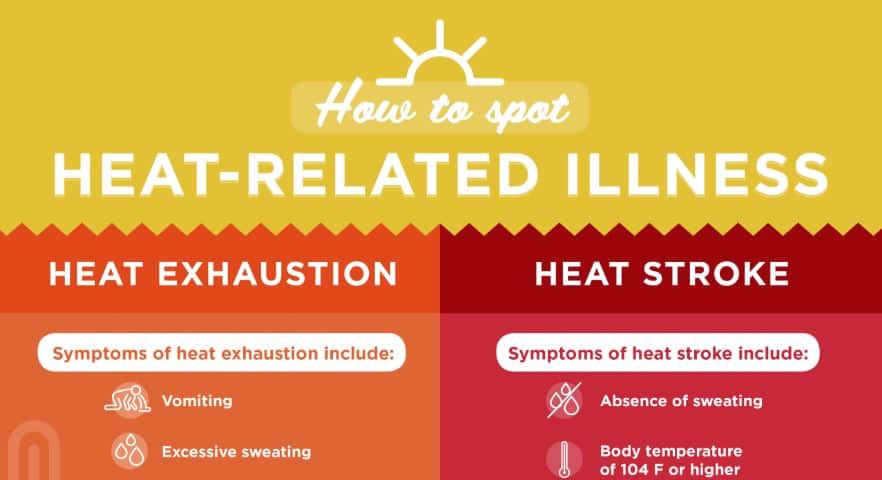
Click on the graphic above to learn more about how heat exhaustion and heatstroke differ.
The next stage is heat exhaustion, often characterized by muscle aches, joint pain, vomiting, diarrhea, fatigue, and headaches.
“Heat exhaustion looks like the flu,” Dr. Simonson says. “You don’t recognize it until you feel poorly. You can get into trouble very quickly.”
Overheating is hard on internal organs, primarily the kidneys and liver, and seniors with heat exhaustion are often admitted to intensive care.
If left untreated, heat exhaustion can progress to heatstroke, which is often fatal.
“With heatstroke, you lose the ability to think and go into multi-system organ failure,” Dr. Simonson says. “Heatstroke carries high morbidity and mortality rates.”
Warning signs include confusion, dizziness, throbbing headache, a body temperature over 103°F, a rapid pulse, and hot, red, damp, or dry skin.

DRUGS CAN CONTRIBUTE
A surprising array of drugs are hypohidrotic, meaning they hamper sweating. They include drugs like dimenhydrinate (Dramamine) and diphenhydramine (Benadryl), along with many medicines used to treat chronic conditions.
“The majority of people in this age group are on multiple meds,” Dr. Simonson says. “Some of these reduce our ability to sweat, and that is the way that we cool ourselves off.”
That said, don’t stop taking maintenance medications just to beat the heat. Consult a doctor if you’re worried about these side effects.
These drugs can compound the effects of heat on the body:
- Dehydration: Diuretics — medications that flush sodium and water from the body through urine — can make you more vulnerable to dehydration. That’s because these medications can make you urinate more than normal. Physicians often prescribe diuretics to treat high blood pressure or swelling caused by kidney disease or other medical conditions.
- Hyperthermia: During hot weather, you have a higher risk of your body temperature rising to a dangerously high level — a condition known as hyperthermia — if you take medications to treat dementia, post-traumatic stress disorder, and generalized anxiety disorder, among other conditions.
- Photosensitivity: A variety of prescription and over-the-counter medications can make your skin extra sensitive to the sun’s ultraviolet rays. These medications include certain antibiotics, antihistamines, diuretics, statins, oral contraceptives, and nonsteroidal anti-inflammatory medications, according to the U.S. Food and Drug Administration. Photosensitivity can cause rash- or sunburn-like damage to your skin (known as a phototoxic reaction) or a true skin rash (photo-allergic reaction).
Avoid anti-inflammatory drugs such as aspirin and acetaminophen if heatstroke is suspected. They won’t help lower body temperature like they do with a common fever.
HOW TO TREAT THE HEAT
The ideal treatments for heat illness are preventive because once exhaustion and heatstroke set it, seeking emergency help tends to be the safest option, especially for older adults.
To avoid heat illness when outside or inside without air conditioning, stay hydrated with water combined with electrolyte solutions such as Pedialyte or Gatorade and take breaks in the shade or air conditioning.
Drinking gallons of water alone can be dangerous because it can wash electrolytes out of the blood, leading to cramps and an accelerated heart rate.
If you lack access to air conditioning, wetting the skin with water and sitting by a fan will help in the short term. If it fails to lower a rising body temperature, go to the emergency department.
Once there, the ER staff can stabilize heatstroke and treat patients with ice packs and cooling fluids with electrolytes delivered intravenously.
“If you feel like you’ve got the flu in the summer, you need to call 911 or go the ER,” Dr. Simonson says. “At 62, 72, 82, you need emergency help.”