A false alarm years ago in a hospital ER made Gary Cannon think twice about calling 911 last fall when his chest pain turned out to be something far more serious.
“Back in 2020, it was nothing more than acid reflux,” Gary says. “The doctors kept trying to reassure me, ‘You need to come see us regardless.’”
The 76-year-old from west Oak Cliff would heed that advice in November 2024, when he returned to Methodist Dallas Medical Center after a blocked artery triggered a heart attack.
“I can’t say enough about the people that helped me,” Gary says. “I could tell they truly cared about whether I made it or not.”

TRUE OR FALSE
The retired computer programmer vividly remembers the day of his false alarm when a bad case of heartburn led him to ask a friend to drive him to the Methodist Dallas ER in August 2020.
“I get paranoid when I have any kind of chest pain,” says Gary, who needed a stent to open a blocked artery in 2015. “It turned out to be nothing, and in the back of my mind I carried that embarrassment that I wasted all those resources at the hospital.”
That feeling still weighed on him before his next visit to the ER last fall, when he woke up in misery with crushing chest pain.
“I could barely breathe—I was having trouble even getting out of bed,” Gary says. “I took a shower, got dressed, and started debating whether I should call 911, which I had never done before.”
‘VERY SERIOUS’
It’s good that he did because Gary would learn from his cardiologist that his heart might have been damaged beyond repair had he waited longer.
“In the cardiology world we say, ‘time is muscle,’” says Nasser Khan, MD, director of cardiology at Methodist Dallas. “When someone has a heart attack, the sooner we’re able to open up the blocked artery, the better your chances of survival and heart muscle recovery.”
Paramedics quickly arrived at Gary’s home and rushed him to the hospital, all while staying in constant communication with the ER team at Methodist Dallas.
“I only live about 3 ½ miles from Methodist, and I could hear the lead paramedic talking to someone on the cell phone, talking about me and my EKG. I was a little out of it, but it all seemed very serious.”
It turns out the ER staff and cardiac catheterization team were arranging a welcome party for Gary: a dozen medical professionals who were very serious about their jobs, too.
From prevention to advanced procedures, trust your heart to the innovative, personalized care that Methodist provides. Visit MethodistHealthSystem.org
IT TAKES A TEAM
Once Gary arrived at Methodist Dallas, he was wheeled into the hospital, where he would soon meet Dr. Khan and the rest of his team.
“There were 10 or 12 people standing in the hall just staring at me,” he says. “I asked the paramedic, ‘Are those people here for me,” and he said, ‘Yes, they are.’”
A call from the ambulance crew can summon the STEMI alert team to the cath lab, day or night, says Dr. Khan, who is quick to emphasize that he “cannot do this by myself.”
“By the time Gary hit the door, I was already down there,” he says, ”and the team was ready to take him right away to the cath lab so that we could open up the blocked artery.”
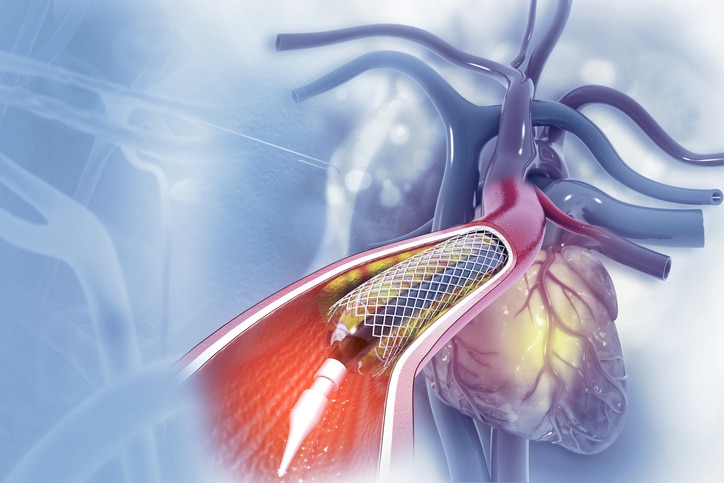
Dr. Khan wasted no time threading a balloon attached to a catheter into his artery, opening the blockage, and leaving a tiny scaffold, or stent, behind to ensure it would stay open.
Throughout the procedure, Gary was comfortably awake and amazed by the efficiency of the team that surrounded him.
“Everybody had their job,” he says, “and they were not messing around.”

TWO MORE STENTS
Three days later, Gary was discharged from the hospital, feeling much better and contemplating his next steps, including the possibility of bypass surgery.
“They told me I had three choices: medication, more stents, or open-heart surgery,” he says. “Bypass surgery just did not sit well with me. To his credit, the surgeon did not pressure me in any way, shape or form.”
During a follow-up appointment in January 2025, Gary got the lifeline he was hoping for from Dr. Khan.
“He said in looking at the scans he could use more stents to open the blockages,” Gary recalls. “He asked if I could come back five days later, and I said, ‘Absolutely, I’ll be there!’”
So on January 27, 2025, Gary returned to the cath lab to get two more stents, along with balloon angioplasty to reopen the stent that was placed in 2015. Gary would go home again the next day to recover and marvel at all he had been through.
“Again, the staff was just unbelievable,” he says. “I absolutely adore them all. I mean, they saved my life.”






