Last year, you either knew someone with COVID-19 or caught it yourself. Now it seems we all know a “breakthrough” case — someone who has been vaccinated but got sick anyway.
Blame the Delta variant, a highly contagious mutation of the coronavirus, because now it’s no longer a choice between getting the vaccine or getting sick.
“Delta just put a spin on that,” says Les Cler, MD, FACP, CPE, the chief medical officer of Methodist Dallas Medical Center. “Now, it’s get vaccinated or you may end up in the hospital.”
TWO DIFFERENT PANDEMICS
Even if you dodge a case of COVID-19, all the pandemic news is enough to give you a headache.
With the Delta variant running wild, case counts and hospitalizations are up. That’s prompted health officials to advise us all to mask up again if we live in areas with low vaccination rates, most of Texas included. Meanwhile, more employers are adopting vaccine mandates.
It’s hard to know whether it’s time to panic or not. So here’s a simple way to put the news about breakthrough infections into perspective:
The pandemic is on two tracks now:
- For the unvaccinated — both here and abroad — the crisis is real and perhaps more serious than it was before because the Delta mutation is so much more contagious.
- For the vaccinated, this year may resemble our future living with the coronavirus. We may catch a nasty cold, but the vaccines will largely spare us from the virus at its worst.
“The vaccines are very good at preventing death and hospitalization, even with Delta,” Dr. Cler says. “Almost all of the most serious cases are among the unvaccinated.”
So are these breakthrough infections among vaccinated people contributing to the rise in cases, or does the blame for the current surge lie with the unvaccinated? The great majority of cases involve the unvaccinated, but let’s save most of the blame for Delta.
“The Delta variant, in particular, has kind of changed the calculus on how careful people who are vaccinated should be in the coming months,” Dr. Cler says.
DELTA FUELS RISE IN CASES
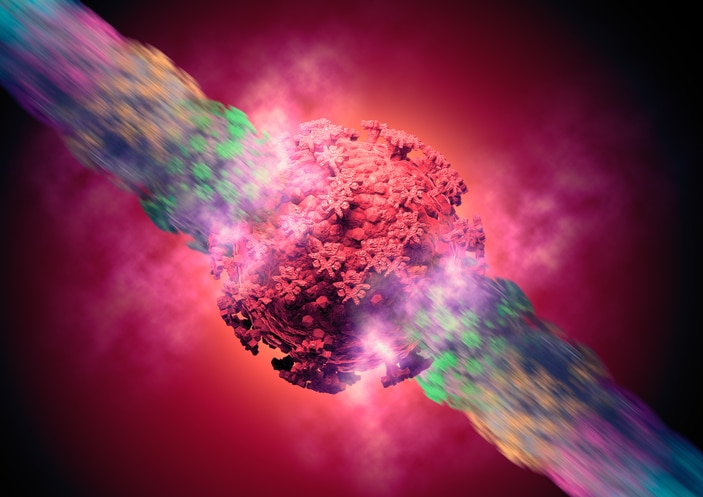
Think of the Delta variant as the “fastest and fittest” version of the coronavirus so far. That’s how health experts around the world have described the mutation, which first emerged in India.
“It’s probably 50% more contagious that Alpha,” Dr. Cler says, referring to the strain that first tore through Britain and was the dominant strain in the U.S. before Delta came along. “And Alpha was 50% more contagious than the original. That puts you at a little over two times as contagious as the original.”
Also, Delta’s incubation period is shorter, four days instead of six, meaning anyone infected with the variant will become contagious sooner, potentially infecting five other people, on average, compared with two or three other people in the early days of the pandemic.
Researchers studying the Delta variant also estimate that it packs 1,260 times the viral load of the original virus. And while a higher viral load may not make you sicker, you will have far more viral particles to shed and infect others.
And the more virus we’re exposed to, whether vaccinated or not, the more likely it is that germ will dodge our defenses and make us sick.

WHO SHOULD BE CAUTIOUS?
Rising case counts this summer have sown doubts about the effectiveness of the vaccines, but nothing has changed: The Pfizer, Moderna, and Johnson & Johnson vaccines are all remarkably good at protecting us against severe infections.
“This is really important for everybody to remember,” Dr. Cler says. “Every vaccine available is at least 93% effective against death or hospitalization from COVID-19.”
No vaccine is 100% effective, and the protection against mild to moderate COVID-19 and an infection without symptoms will be lower, especially with more infectious variants circulating.
That’s no reason to panic, but it’s a good reason to be cautious, especially in areas where vaccination rates are low. That explains why the CDC recently changed its guidance on mask-wearing for the vaccinated.
“If you go into a crowded area with low vaccination rates, especially indoors, you really need to think critically about what’s going on,” Dr. Cler says. “Because even if you’re vaccinated, think about those who aren’t. Maybe you have children or immunocompromised people in your own household who are still vulnerable.”
So while you may be vaccinated and well-protected against a severe case of COVID-19, there’s still a chance you could catch a less serious case and spread the disease, causing a severe infection in the millions of Americans who remain vulnerable.
For now, it would be wise to put your guard up again and resume the same precautions that helped us flatten the curve before. This includes wearing a mask, watching your distance, and washing your hands.
VACCINES ARE THE SOLUTION
All those tried-and-true precautions will only take us so far, however. Health officials agree there’s only one reliable way to end the pandemic: raising vaccination rates.
We don’t need to eliminate the coronavirus to get back to normal. Most experts have given up on the idea of reaching herd immunity after the rise of highly contagious variants.
But getting more people vaccinated will go a long way toward putting the virus into a corner and leaving it with far fewer vulnerable hosts to infect and spread.
“The sooner everyone is vaccinated, the sooner we climb out of this,” Dr. Cler says. “We’re going to save more moms, dads, grandmas, grandpas. People that somebody loves.”


