Influenza and the common cold barely surfaced at the height of the pandemic, thanks to mask use and social distancing. That was fortunate because COVID-19 was raging at the time and the U.S. dodged a potentially disastrous “twindemic.“
But this fall, cold and flu viruses are making another comeback, as many people cast their masks aside and share breathing space again. And the rest of 2022 into early 2023 could be even worse if flu season surges and creates a potential “tripledemic.”
“If we end up seeing simultaneous infections with COVID-19, influenza, and RSV, the situation could become complicated,” says Leigh Hunter, MD, FACP, an infectious disease specialist and director of the Methodist Internal Medicine Residency Program.
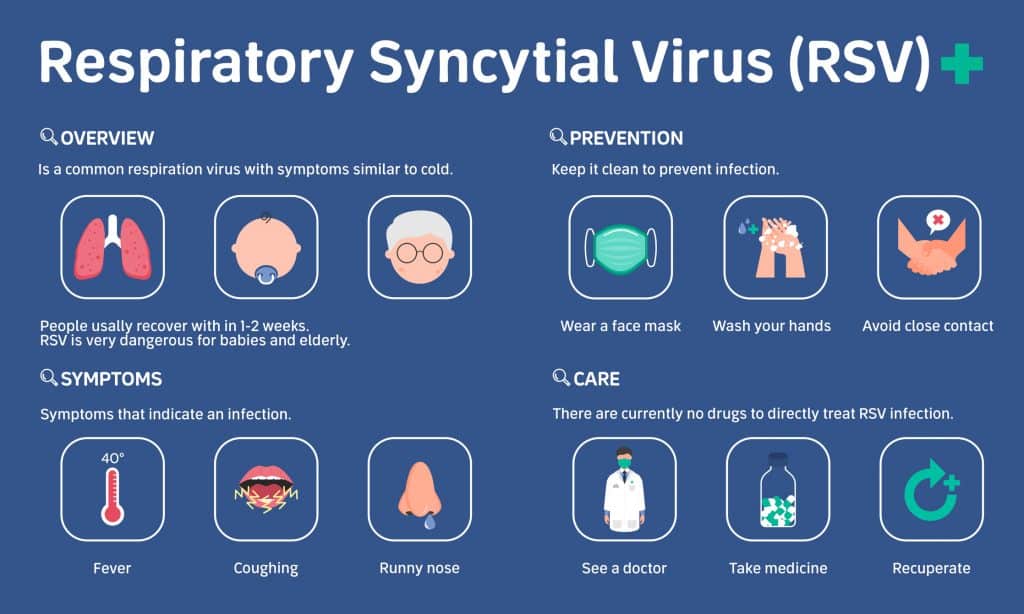
Young children and seniors are especially at risk right now because one of the biggest threats is respiratory syncytial virus, a nasty cold commonly known as RSV.
“RSV threatens the very young, the very old, and the immunosuppressed,” Dr. Hunter says.

WHAT IS RSV?
For most of us, RSV causes a nasty cold, but for children under 1-year-old, it’s the most common cause of pneumonia and bronchial infections.
Such an infection can become dangerous if it spreads to the lower respiratory tract and causes bronchiolitis, an inflammation of the tiny airways in the lungs. Symptoms start out similar to the common cold but can progress to coughing, wheezing, and difficulty breathing. Older adults are also at risk, as are people with heart or lung disease and anyone with a weak immune system.
RSV infections typically surge in the fall and winter. But the 2020-21 and 2021-22 cold and flu seasons were barely a blip because of social distancing, mask mandates, and widespread virtual learning.
Now those viruses are playing catch-up, especially among young children who haven’t experienced the usual respiratory viral infections, Dr. Hunter says. Babies born in 2019 through 2021 may have never been exposed to RSV, and they are fertile ground for a virus that has no vaccine.
“With decreased circulation, there has not been the usual exposure and level of community immunity,” she says.
HOW TO SPOT RSV
Telling the difference between an RSV infection and COVID-19 can be a challenge, Dr. Hunter says. Also, both viruses can occur together. If your child catches RSV, it may lower their immunity and put them at higher risk for a COVID-19 infection, and vice versa.
That’s why you should visit a doctor, especially if your symptoms, or your child’s, become severe or won’t go away after one or two weeks.
“We need to do testing with a respiratory virus panel that looks for RSV, COVID-19, and other viruses,” Dr. Hunter says.
The worst symptoms of RSV include difficulty breathing and a high fever. Children and older adults can also develop a blue pallor to the skin, especially the lips and nail beds.

WHAT ABOUT THE FLU?
RSV is surging now, but the flu could be our next problem, especially if it re-emerges alongside a new COVID-19 variant. So while we may have avoided it in 2021 and 2022, a “twindemic” or even a “tripledemic” remains a real possibility.
The Centers for Disease Control and Prevention reports the percentage of patients testing positive for flu nationwide hit 4.4% in late October 2022, compared with 0.1% at the same time in 2021. That’s still relatively low, the CDC says, but it’s a worrisome increase (especially so in Georgia and Texas) and suggests flu season could strike early this year.
In the 2021 flu season, the CDC says there were only a few thousand cases of flu reported nationwide — down from more than 200,000 in an average year.
That was the lowest level on record, and it makes developing a flu vaccine far more difficult because there’s less data for researchers to draw on to predict which strains will be prevalent in the fall.
Of course, that’s no reason to skip the flu vaccine when it becomes available. And it’s possible by next fall, there will be a vaccine that kills two bugs with one stone.
“Research is underway to combine the flu and COVID vaccines, which looks promising,” Dr. Hunter says.