Fighting for his life is nothing new for Steven Pratt, a Vietnam veteran who recently took up boxing to battle Parkinson’s disease. So it’s no surprise that when he found out he needed a lifesaving heart surgery, the 81-year-old tackled it head on.
“I had faith that the good Lord was going to take care of me,” he says. “He hasn’t failed me to this point in time, and I didn’t feel that he would drop the ball now.”
Steven, a retired child psychologist who ran a Catholic charity in Denver before moving to Texas, found the care he needed at Methodist Southlake Medical Center, where a cardiologist diagnosed him with aortic stenosis, a potentially fatal narrowing of the heart valve.
“I woke up one morning with a really rapid heartbeat and had trouble breathing,” he recalls. “I ended up going to the emergency hospital nearby, and they said I either was having or had a heart attack.”
Steven was taken to Methodist Southlake, where he was diagnosed by Anas Alomar, MD, medical director of the cardiology department on the medical staff at Methodist Southlake.

UNDER A WATCHFUL EYE
Steven was not having a heart attack, Dr. Alomar determined, but he did have atrial tachycardia, a too-rapid heart rhythm that causes the upper chambers of the heart to beat faster than the lower chambers.
The cardiologist decided to monitor Steven’s condition for about a year, regularly evaluating his heart rhythm and valve function with heart rhythm monitors, echocardiograms, and regular clinical exams.
“Over time, it became clear that his aortic valve was progressively narrowing and his symptoms — fatigue and shortness of breath — were consistent with severe aortic stenosis,” Dr. Alomar says. “That’s when we determined that replacing the valve was the appropriate next step.”
Dr. Alomar underscores how critical early detection was in Steven’s case.
“Severe aortic valve stenosis carries a significant risk of sudden death, especially in individuals with symptoms,” he says. “Without treatment, the average survival rate for patients with symptomatic severe stenosis is around two to three years.”

TAVR TO THE RESCUE
For Steven, that treatment would come in the form of a transcatheter aortic valve replacement, or TAVR, a minimally invasive procedure performed at Methodist Richardson Medical Center.
This minimally invasive procedure uses an artificial implant to replace a narrowed aortic valve that isn’t functioning properly, usually because of age-related wear and tear and calcification of the valve. Using a catheter, a doctor can place the new heart valve through an artery in the leg.
“Years ago, valve replacement surgery was an open-heart surgery,” says Derek Williams, MD, cardiovascular surgeon on the medical staff at Methodist Richardson. “Now we can replace the valve using a catheter, and the patient goes home the next day.”
Steven had his TAVR in November 2024, and the procedure immediately allowed his heart to pump blood more effectively, leading to improved energy levels, less shortness of breath, and a better overall quality of life. He felt well taken care of every step of the way.
“I still marvel at the ease with which the procedure was done,” he says. “It’s hard to put my feelings into words — being able to have a valve run up my leg and into my heart to fix the issue is just short of a miracle.”

BACK TO BOXING
Steven saw tremendous results quickly, noting that after just two days he saw a major change in his energy and has returned to normal activities with fewer limitations, pastimes that include playing the trumpet and boxing.
“I box twice a week in an organized program for Parkinson’s patients,” he says. “Each boxing session is an hour long, and now I believe I’m more capable of participating because of the heart valve.”
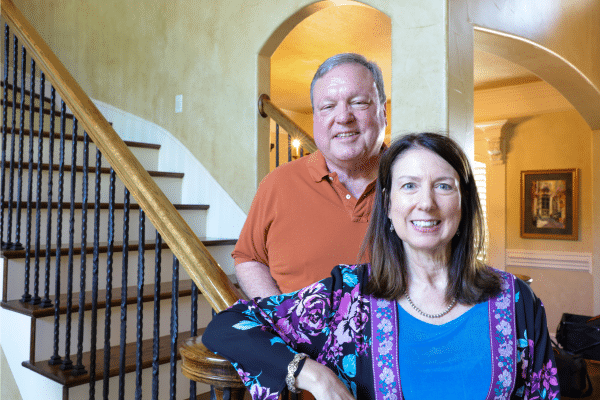
Today, Steven and his wife of 56 years, Bernice, are enjoying retirement in Texas, staying active with their grandsons’ school and sports activities. The trained psychologist credits his family for helping him recover mentally.
“The strength of family was a large part of the psychological recovery,” he says.
Looking back, Steven encourages others not to delay care and feels blessed to have addressed his heart disease in time.
“Before the surgery, I had a lot of fatigue, and that slowly creeps up on you. You start to think it’s just normal,” Steven says. “After surgery, the difference in my energy and enthusiasm is marked.”