Lower back pain catches up with almost everyone — up to 80% of Americans by some estimates — but the causes can range from muscle strains to arthritis and herniated disks. And in the case of a slipped disk, the pain might not be in your back at all.
“If you have a herniated disk, or a bulging disk, sometimes the pain does not seem to come from the back,” says Lauren Sand, MD, neurosurgeon on the medical staff at Methodist Richardson Medical Center. “Instead people describe it as an electrical or shooting pain down the back of the leg.”
A primary care doctor can help distinguish run-of-the-mill back pain from a slipped disk, and Dr. Sand notes three red flags when you should get help right away.
“Seek urgent medical care if you’re having any sudden weakness, urinary or bowel incontinence,” she says. “If the pain or numbness alone is affecting your quality of life, this is also a very good reason to seek medical attention.”
SHOCK ABSORBERS
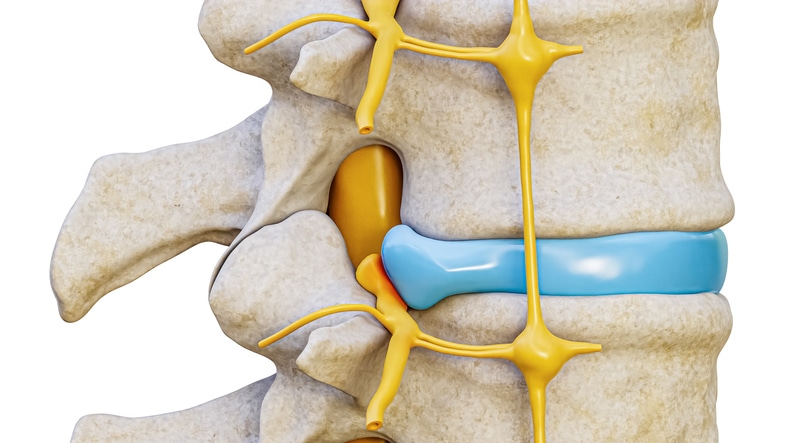
There are gel-like cushions between the 24 vertebrae in our cervical, thoracic, and lumbar spine, and any one of these disks can rupture, either with age or because of a traumatic injury such as a car crash.
The trouble starts when these shock absorbers slip out of their usual confines and push against the bundle of nerves surrounding our spines, causing pain, numbness, or tingling.
“If that happens, it can pinch the nerves that travel to important areas of the body,” Dr. Sand says, “and that may be why you start having the symptoms you’re having.”

SCIATIC NERVE PAIN
If a disk ruptures in your neck, you could feel it in your arm, chest, or even abdomen.
“It’s quite common in the neck and lower back,” Dr. Sand says, “less so in the middle of the back because you’re not moving that as much as your neck and lower back, which are more prone to degenerative changes.”
Five of these disks are in the lumbar region, or lower back, which carries the biggest burden when we move around or sit slouched in a desk chair for hours on end.
When a disk ruptures in your lower back, it may push against the sciatic nerve, the longest nerve in your body, which travels through the hip and backside all the way down the leg.
The resulting pain, tingling, or numbness — commonly referred to as sciatica — can be severe and even weaken the affected leg or cause bowel or bladder problems.
“The majority of the time, conservative measures such as physical therapy and anti-inflammatory medications will solve the problem,” Dr. Sand says. “Occasionally it doesn’t get better, which is often an indication that surgery could be the better option.”

DIAGNOSIS AND TREATMENT
The first step to relieving chronic back pain is to see a doctor, whether it’s a primary care physician or a specialist. They will likely start with an X-ray or a CT scan to ensure that there are no fractures or other serious problems.
But these tests usually can’t detect a herniated disk or nerve issues. For that, you’ll need an MRI.
“CT scans and X-rays are mostly for looking at bone,” Dr. Sand says. “An MRI is a unique tool that can clearly define disk spaces, nerves, the spinal cord, and other surrounding soft tissue.”
Once the problem disk is diagnosed, most doctors will opt for conservative measures, like over-the-counter pain relievers, back stretches, and alternating cold packs and hot pads.
If the pain doesn’t go away within a few weeks, a doctor may prescribe anti-inflammatory drugs or muscle relaxants, and eventually, turn to physical therapy.

WHEN TO CONSIDER SURGERY
Surgery may become necessary if the pain is severe enough and has not dissipated, or if it is significantly affecting daily living.
“For example, surgery may be the best option if it’s a large disc herniation that’s unlikely to get better on its own,” Dr. Sand says.
And again, she emphasizes, watch for those red flags: weakness, pain that disrupts your daily life, and incontinence. Don’t wait to seek help in those cases.
“Bring it forward to your primary care provider if you have any concerns,” Dr. Sand advises, “and then they can help guide you in the right direction, whether it is a nonsurgical or surgical route.”

